Chances are that if you found my website you already know a little something about diabetes. But, you might be like me and always want to learn more. And there's ALWAYS is more to learn about diabetes. In this page/post I will attempt to give you my interpretation of diabetes. But I will also refer to medical people who can get more technical. I will also talk about the symptoms of diabetes, the risk factors and different types of diabetes.
Diabetes is not easy to explain and it usually requires more than a short sentence, which means people's eyes glaze over and you lose them before you get to the "good" stuff. But you still have to try right.
It's important for all of us, people with diabetes, to not only explain our type correctly but when we are asked about other types that we support those people well too.
Let's start with the basics. Most of the medical definitions I've used here came from the Canadian Diabetes Association's website.
Diabetes is;
Diabetes is a lifelong, chronic, and sometimes fatal disease about the struggle to manage glucose levels in your bloodstream. The body either cannot produce insulin or cannot properly use the insulin it produces.
What do we need insulin?
Insulin is a hormone that turns the glucose (sugar) in our blood into energy for all of our cells to function. The glucose comes from a couple of sources, mostly from foods known as carbohydrates and a stored supply in our liver. Diabetes leads to high blood sugar levels, which can damage organs, blood vessels and nerves - every where our blood goes means that's an area excess sugar can damage. - See more here.
There are a bunch of different types of diabetes.
Type 1 Diabetes
My (non scientific, non-medical) description; Type 1 diabetes happens when, for some unknown reason, our immune system goes "terminator" on our insulin making cells and wipes them all out. My body now has no way to convert the food I eat, in particular the good stuff that comes in the form of carbohydrates, into fuel for my body to exist. Or the glucose that is constantly being released from my liver to keep energy levels up in between meals.
About five to 10% of people with diabetes have type 1 diabetes and it can happen at any age. Type 1 diabetes generally develops in childhood or adolescence, but can develop in adulthood. And type 1 diabetes is always treated with insulin."
For the more medical explanation of type 1 diabetes click here. "The risk factors for type 1 diabetes are still being researched. However, having a family member with type 1 diabetes slightly increases the risk of developing the disease. Environmental factors and exposure to some viral infections have also been linked to the risk of developing type 1 diabetes." Source - International Diabetes Federation (IDF)
Symptoms of Type 1 Diabetes:
The symptoms of type 1 diabetes can develop very quickly (over a few days or weeks), particularly in children.
The main symptoms of type 1 diabetes are the 4T's :
- Excessive Thirst
- Excessive trips to the Toilet
- Excessive Tiredness
- Thin; losing an excessive amount of weight
Other symptoms can be vomiting or heavy, deep breathing can also occur at a later stage. This is a dangerous sign and requires immediate admission to hospital for treatment. For more information on the symptoms of type 1 diabetes, click here.
LADA (latent autoimmune diabetes in adults) or Type 1.5
My (non scientific, non-medical) description; LADA is very much like type 1 diabetes but it tends to occur in older adults. It is very often mistaken for type 2 diabetes. It's a slower destruction of the insulin making cells. Maybe it's something to do with the "Terminator" being older and slower moving!?! So the symptoms present over a longer period than they would for a person with type 1 diabetes.
LADA is also known as slow-onset type 1 diabetes and type 1.5 diabetes. Like other forms of type 1 diabetes, people with LADA require insulin injections to normalise their blood glucose levels.
For the more medical explanation of LADA click here. Symptoms are very similar to those of type 1 diabetes.
Type 2 Diabetes
My (non scientific, non-medical) description; Type 2 diabetes happens when your insulin has developed a dementia. It's old and tired and not quite sure what it's suppose to do. So, sometimes it works and sometimes it has to put twice as much effort in to work. To me, it's like the insulin has dementia - sometimes it's sharp and works well and other times it just can't figure out what to do.
In general, people who develop type 2 diabetes are older but this isn't always the case. it's the most common type of diabetes.
The treatment options for type 2 diabetes include managing physical activity and meal planning, or may also require medications and/or insulin to control blood sugar more effectively. It can be a series of trial and error to find the right treatment plan for a person with type 2 diabetes.
For the more medical explanation of type 2 diabetes click here.
Symptoms of Type 2 Diabetes:
The symptoms of type 2 diabetes can be very slow to present and often you can have type 2 diabetes for a number of years before it is picked up.
The most common symptoms of type 2 diabetes include:
- excessive thirst
- frequent or increased urination, especially at night
- excessive hunger
- fatigue
- blurry vision
- sores or cuts that won’t heal
Risk Factors for Type 2 Diabetes (from IDF):
There are 10, that's TEN risk factors for type 2 diabetes. Not just the two/three that we ALWAYS hear about.
- Family history of diabetes
- Increasing age
- High blood pressure
- Ethnicity
- Impaired glucose tolerance (IGT)*
- Overweight
- Unhealthy diet
- Physical inactivity
- History of gestational diabetes
- Poor nutrition during pregnancy
Impaired glucose tolerance (IGT) is a category of higher than normal blood glucose, but below the threshold for diagnosing diabetes.
Gestational Diabetes
The other description from IDF; is a form of diabetes consisting of high blood glucose levels during pregnancy. It develops in one in 25 pregnancies worldwide and is associated with complications to both mother and baby. GDM usually disappears after pregnancy but women with GDM and their children are at an increased risk of developing type 2 diabetes later in life.
Approximately half of women with a history of GDM go on to develop type 2 diabetes within five to ten years after delivery.
Other Types.
There are other, much rarer forms of diabetes that are monogenic, meaning a change in only one gene is responsible for the condition. There are two types of conditions in this category: Maturity Onset Diabetes of the Young (MODY) and Neonatal Diabetes Mellitus (NDM).
For these types of diabetes I have to call on the words of experts because I'm not very familiar with them and don't feel comfortable giving a description of something I don't know much about.
MODY Maturity Onset Diabetes of the Young
I would love to take credit for this explanation of MODY but I couldn't do any better than Morag (Twitter: @SparklyRedShoes) on GBDOC ; MODY happens when there is a mutation of a gene and is most often hereditary. It very often is confused as type 2 diabetes in a young person.
"MODY is diagnosed by genetic testing. It may be worth testing for MODY when a person with diabetes doesn’t fit the profile of the more usual types. For example, somebody who actually has MODY may not require as much insulin as most people with Type 1 (and will have measurable C-peptide), even long after the honeymoon period, but they will generally not be of the age and weight you might expect to see for Type 2. In fact, at diagnosis, people with MODY are often young, slim and active. "
Being genetic, it runs strongly in families; if one parent has it, then the chances of a child inheriting the gene are 50/50. People with a MODY gene generally develop diabetes as young adults, and most are diagnosed by age 45.
For the more medical explanation of type 2 diabetes click here.
The key features of MODY are;
- Being diagnosed with diabetes under the age of 25.
- Having a parent with diabetes, with diabetes in two or more generations.
- Not necessarily needing insulin.
NDM Neonatal Diabetes Mellitus
 From Diabetes UK; Neonatal diabetes is a form of diabetes that is diagnosed under the age of nine months. It’s a different type of diabetes than the more common Type 1 diabetes as it’s not an autoimmune condition (where the body has destroyed its insulin producing cells). Like MODY it's a genetic mutation.
From Diabetes UK; Neonatal diabetes is a form of diabetes that is diagnosed under the age of nine months. It’s a different type of diabetes than the more common Type 1 diabetes as it’s not an autoimmune condition (where the body has destroyed its insulin producing cells). Like MODY it's a genetic mutation.
The key features of neonatal diabetes are:
- Neonatal diabetes is caused by a change in a gene which affects insulin production. This means that levels of blood glucose (sugar) in the body rise very high.
- The main feature of neonatal diabetes is being diagnosed with diabetes under the age of 6 months, and this is where it’s different from Type 1, as Type 1 doesn’t affect anyone under 6 months.
- As well as this, about 20 per cent of people with neonatal diabetes also have some developmental delay (eg muscle weakness, learning difficulties) and epilepsy.
- Neonatal diabetes is very rare, currently there are less than 100 people diagnosed with it in the UK.
- There are two types of neonatal diabetes – transient and permanent. As the name suggests, transient neonatal diabetes doesn’t last forever and usually resolves before the age of 12 months. But it usually recurs later on in life, generally during the teenage years. It accounts for 50-60 per cent of all cases. Permanent neonatal diabetes as you might expect, lasts forever and accounts for 40-50 per cent of all cases.
- Around 50 % of people with neonatal diabetes don’t need insulin and can be treated with a tablet called Glibenclamide instead. These people have a change in the KCNJ11 or ABCC8 gene and need higher doses of Glibenclamide than would be used to treat type 2 diabetes. As well as controlling blood glucose levels, Glibenclamide can also improve the symptoms of developmental delay. It’s important to know if you have/your child has neonatal diabetes to make sure you’re/they’re getting the right treatment and advice (eg stopping insulin).
- Genetic testing for neonatal diabetes is offered free of charge for all people diagnosed with diabetes before 9 months of age. Confirming the diagnosis by molecular genetic testing is essential before considering any change to treatment.
- More information about neonatal diabetes can be found here.
So if you were/your child was diagnosed with diabetes before you/they were 6 months old, ask your diabetes team for a test for neonatal diabetes. Your team can take a blood sample and send it to the Peninsula Medical School based at the Royal Devon and Exeter Hospital for analysis. The test is free. Go to www.diabetesgenes.org. This site will also tell your doctor how to take your blood and send it to the team at Exeter.









 From
From 


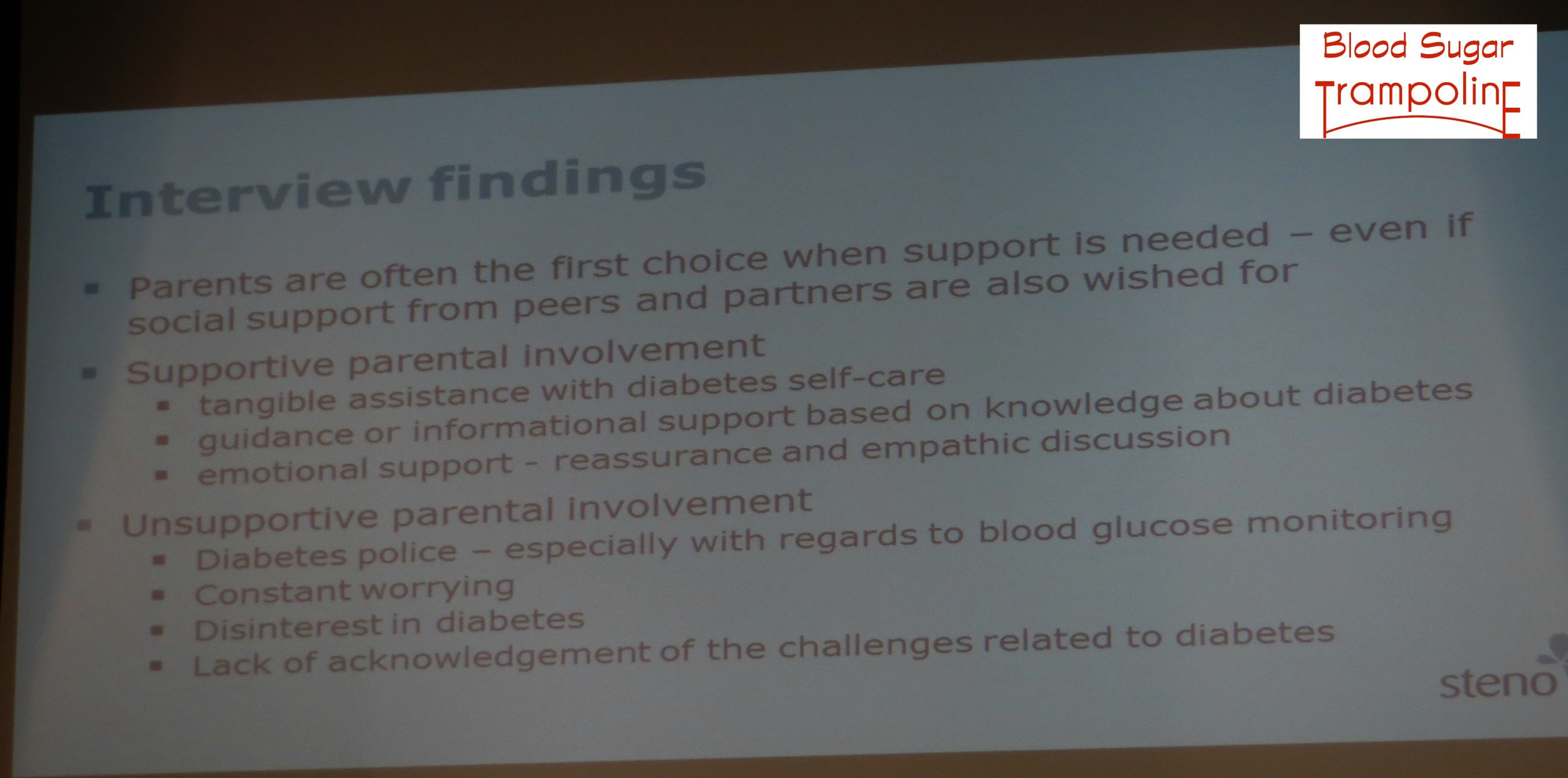 Emerging adults do not want to be too dependent on their parents - they want parents to be available when needed.
Emerging adults do not want to be too dependent on their parents - they want parents to be available when needed.