In this post, I will provide a short summary of the information revealed from parliamentary question responses on how many people in Ireland use insulin pumps, what clinics provide them as a treatment option and how many new pump starts are done each year.
Making Sense of the Glycaemic Index
Mid October, I went to the DiabetesSisters Weekend for Women conference Alexandria, Virginia. See disclaimer at the end. One of the outstanding presentations I attended was by Thriveabetes 2016 speaker, Gary Scheiner’s presentation on “Making use of the Glycaemic Index”. This should not be a surprise to anyone has read Gary’s book “Think Like a Pancreas”. I will be honest here; when I heard the words “Glycaemic Index” I pretended I didn’t. And the reason is that several years ago, when it became a thing that was relevant to diabetes management, I tried to learn but I found it completely and utterly confusing. So I went to Gary’s talk as a skeptic.
BUT! As always Gary puts the information together well. See his blog posts here.
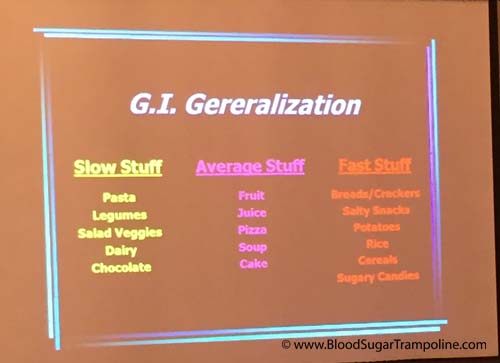
He started by saying that the glycemic index is the speed glucose enters the blood in the first two hours. It does not measure how fast foods enter the blood as glucose beyond that or how long it takes at all. A-ha! Ok so glycemic index is useful information for first two hours. I feel exonerated now.
This is hugely relevant to my diabetes management because I know that my rapid acting insulin peaks in approx 2 hours and that I might need additional insulin doses after that to cover the glucose released into my blood after the two hours.
The glycemic index is measured from 0 to 100. The closer to 100 a Food is, the higher its glycemic index is and the quicker the glucose hits your blood.
Here is a snapshot of the other things I learned;
- A mixed meal, ie a meal with protein, carbohydrates and or fat gravitates towards the carb. Meaning your body will process that first, albeit slower than if it was just carbs. So I might need to take a post meal dose of insulin in addition to my pre-meal dose.
- If you have a low GI food before your meal it will slow down the follow up starch in your meal. This is really good to know! Bring on the peanuts before the pasta or pizza :-)
- Larger portions take longer to digest. This isn’t new information to me but I suppose I always underestimate just how flippin’ long it takes.
- Time since your last meal affects the glycemic index. If you are still processing your food from the last meal, it’s going to slow down glucose absorption even more.

Some additional pieces of information not related to glycemic index but valuable.
- Don’t trust your CGM when you are recovering from a low. The lag time in full force.
- Insulin on board pump feature doesn’t take into account the food on board. As mentioned in the previous paragraph, if you are still digesting food you may need to override the insulin on board recommendation.
- Insulin resistance can happen if you have a meal with a lot of fat.
- Protein to insulin formula = ½ The total of protein grams and treat as carbs.
- Amylin/Symlin is a hormone that slows gastric emptying. People who don’t have insulin don’t have amylin either so stomachs process food quicker.
- Victoza is a GLP-1 injectable medication and reduces glucagon secretion; slows down the absorption of food.
In summary, glycemic index important to people with diabetes because:
- Satiety. Low glycemic index meals help you feel full for longer.
- Helps with the Timing of insulin. For example, if you know a meal or snack is going to have a high glycemic index then you could take your insulin 15 - 20. Minutes beforehand to give it a head start.
- Helps avoid post meal spikes
So, I’m glad that I learned all of this and I’m glad that I don’t have to waste any more of my time trying to figure it out because it makes more sense to me now. And It may help me to know the glycemic index of a Food I’ve never tried before so that I can figure how to deliver my insulin (pre-meal, at meal or extended Bolus).
Disclaimer: Diabetes Sisters paid for my conference registration and accommodation but also gave me a contribution towards my travel costs. All they asked for in return was that I would write a blog post about the conference which I had to do anyway because I learned so much that needs to be shared;-) And I wrote here about how I was selected.
Diabetes on steroids
Back in October, I had a steroid injection in my hip. And yes, it drove my glucose levels bananas! For those of you who may not be aware of it, steroids are one of the medications that truly mess up glucose numbers for lots and lots of people. The ultimate craziness only lasted two to three days but the residual crazy lingered a couple of weeks.
Here’s a little of the backstory behind why I got a steroid injection.
I have been complaining about my right hip for some time and I finally did something about it in September 2016. I went to my GP. He referred me to my physiotherapist and we did some “process of elimination” exercises. They didn't work. So then I went for an MRI and was referred to a rheumatologist.
At least now, we think I know what is wrong with my hip! It would seem both my physiotherapist and my rheumatologist agree that I have bursitis. And my rheumatologist injected steroids to reduce the swelling. If you have diabetes and you have steroids that plays absolute havoc with blood glucose.
However, no one could tell me how many days, weeks, months the glucose madness would go on for and how severe it would be.
Here is my experience of what happened to my glucose levels.
Prior to my injection my diabetes management was going fairly well with just the usual ups and downs. I had the shot mid morning and my glucose levels didn’t feel the effect of the injection until after lunch. But after lunch my numbers remained in the high teens until the early hours of the next morning. On day two, I noticed that if I increase my mealtime insulin significantly more than usual it would keep them in check. However, if I forgot to make the increase then I struggled to bring my numbers back down for hours.
Then the effect of the steroid started to wane slowly over the next two weeks and I had the opposite problem: trying to keep my glucose levels above hypo level. I adjusted insulin doses slowly and only making one or two changes at a time to bring them back to my normal diabetes levels (?!?!).
I was grateful that not only was I aware that this would more than likely happen but that both my endocrinologist, rheumatologist and physiotherapist reminded me it would. I'm probably going to have another dose in January but now, at least, I have a good idea of what to expect.
Weather the diabetes havoc-er
One of the factors not included in Diatribe’s 22 factors that influence glucose levels is the weather. Sometimes the weather plays with my diabetes management. And here’s how. Do you remember that really, really wet day we had last week? It seems like a distant memory now and I don’t think it had a name, like a storm name, but most of the country was flooded under a yellow weather warning.
When I got up that morning and look out the window I thought “Nope, I’m not walking, I don’t mind being wet and drippy but not that wet!” I was disappointed because most days I love my walk. It clears my head as I inhale clean fresh energy and exhale stress. I swing my arms vigorously and loosen up my neck and shoulders. I had missed my walk the day before due to a doctor's appointment so I was doubly disappointed.
So, with my daily constitutional off the menu, I took my “no-walk” breakfast insulin dose, which tends to be twice what I take if I am walking and off I drove the kids to school.
However, as I was dropping the teen and preteen to school the rain wasn’t that bad. So,I changed my mind (GASP)…. but how can I avoid a hypo seeing as I’ve taking all this insulin without using calories to prevent the low glucose reaction that will surely follow?
I decided to turn my background/basal insulin down to zero for one hour on my insulin pump. Yes, it was going to take an hour to take effect but it was better than a severe hypo. At least it might soften the blow.
Now, if I was on injection pens there is no way I could have avoided preventing a low without glucose.
So was I successful? Weeelll, kind of. I did have a hypo. A doosy at 2.8mmols but it didn’t feel as bad as it was and I didn’t feel like I had to consume the entire kitchen just about a dozen small jellies.
Compared to most hypos this one rebounded quite quickly and not too high. However, I did spend most of the day with glucose levels that were more elevated than my usual.
And there you have it, diabetes the spontaneity killer and weather the diabetes havoc-er.
Living with Diabetes is like Parenting
My life is finally slowing down after a number of weeks of events, diabetes awareness "stuff" and children being off school for mid term break. I have so many blogs posts in my head and no time to write them. But soon... In the meantime, while I was fast asleep, my husband had a moment of inspiration about living life with type 1 diabetes and what common human experience might come close to describing the type 1 diabetes experience? Yes, there are a lot of questions to ask about why I was asleep and he wasn't but not for publishing online ;-)
So here is a guest post from my hubby.
Gráinne was away at a conference recently, presenting the "patient experience" to a group of 100 almost entirely healthcare professionals. She came home the first evening very excited by not only how well her talk was received, but the general tone of the conference in general.
1. Say goodbye to a reliable full night of uninterrupted sleep.Even in her pre-CGM days, Gráinne would wake up in the middle of the night not feeling right. Her sugars could be high or they could be low, or she could just be coming down with something. Regardless she had to check her sugars and then decide how to react to the information.I wouldn't say it's quite like having a newborn baby, but it's pretty close to having a 6 month old baby who can't reliably settle. But without the option of seeing if the baby will be able to settle herself...and without the possibility that the 6 month old baby will grow out of it.2. There is no rulebook.A new parent is often desperate for a manual on "how to be a good parent." What you learn as a parent is that every child is unique and has their own set of needs. You just need to figure out what works best for the child in front of you at the time. And of course what works for a two year old is not what works for a twelve year old: the "rulebook" for parenting is forever changing.Type 1 seems to work in much the same way. There are so many variables in life that what worked for you last week may not work for you this week. You just take on whatever challenges type 1 throws at you, and deal with them in the best way your sleep-deprived, hypo-affected brain can manage.3. Frequent guilt.We've all as parents done things that we regretted. Maybe it was giving a punishment that was in retrospect overly harsh. Or maybe we're worried that we're being too lenient, or not helping our child learn lessons the hard way because we're spoon-feeding them the answers. Or maybe our child is struggling in school, or struggling socially, or trying really hard in a sport that they love but are lacking the skills to be really good at...and we feel somehow responsible for this and guilty that we're failing them as parents.If you have type 1, guilt about "not managing your diabetes" seems to be there. Always. That bit of extra chocolate you had because it looked nice? Unless you accounted for it perfectly (and see point 2: you probably didn't account for it perfectly because there is no rulebook), you're probably going to see the result of that "indiscretion" in your blood sugars. Not getting the HbA1c result you hoped for? More guilt and self-loathing.4. Low-grade worry.As parents, we often worry about our children's future. Some of these things are those over which we have control (and feel guilty about doing "wrong"). Others are longer-term things over which we have no real control: is the planet going to be habitable by the time my grandchildren are born? And every so often, we think about our own mortality: what would happen to our children if Gráinne and I were to die unexpectedly?These aren't necessarily things that keep us as parents up at night (those are more the "guilt" topics!), but they are the things that can weigh on the mind of a person with type 1. Mortality is a much more real presence in the life of someone with type 1: the very medication that is needed to keep you alive can also kill you (or worse).5. Lots of "outside" adviceNew parents (and experienced parents!) are often awash in advice, both solicited and unsolicited. It is advice commonly wrapped in "you should" and "never" and "always"...very emotionally charged terms.Have you ever talked to a mother who wants to breastfeed but wasn't able to make it work for whatever reason? Feeding her baby with a bottle can bring on a whole world of emotions with that simple act of providing nourishment to her child, and that's before the very "helpful" commentary from some well-meaning individual: "breast is best!"The world of diabetes management is awash in advice, much of it from medical experts and some of it from crackpot experts who read an article about "how cinnamon can cure diabetes" or some other such thing. But much with parenting, what a PWD must do is learn to figure out what advice is helpful to them and use that, whilst figuring out how to deflect and ignore advice that does not.
The Death of the Animas Insulin Pump
Last week, Johnson & Johnson Diabetes, who own Animas, announced that it was “exiting” out of the insulin pump business, effective immediately in the US and Canada. And eventually in the rest of the world. Once I read all the way down the press release to realise that it was just USA and Canada for now, I was relieved.
Then I was seriously miffed, but not completely surprised. Since the Vibe insulin pump was introduced, a number of years ago, innovation seemed to have stalled within the company. Johnson & Johnson own both Animas and the glucose meter company LifeScan/OneTouch but they didn’t even innovate between these products, not even to do what all others were doing and that was to sync products via Bluetooth or whatever internet cloud magic they choose. One might even say they really checked out of the diabetes industry a long time ago by their lack of interest.
So, what does this mean for us in Ireland? And what does this mean for me an Animas Pump user?
I have been using an Animas pump since my pumping beginnings in 2010. Then in 2014, I upgraded to the Vibe and in 2015 I added the Dexcom Continuous Glucose Monitoring System (CGM) to it. I didn't choose which insulin pump I would have, it was chosen for me, but I didn't have any complaints. In fact, it's been a great relationship!
Now I'm trying to think ahead and I realised that in the not too distant future I'm going to have to find a replacement for my insulin pump.
What are my choices in pumps? Do I actually have a choice, when the only other insulin pump my health service has a contract with is Medtronic? Yes it's probably a good pump but I don't want to be forced into it.
BUT it's not just my pump I need to consider!
This also effects my CGM device. How will my new pump interact with my current CGM, if at all? My Dexcom receiver IS my insulin pump, meaning that my glucose sensor transmits the information straight to my pump. So I need to either get a new receiver device or change CGM’s.
And then, there's my glucose meter which I was also able to upload to my insulin pump software programme which allows me to create useful graphs that help me make better decisions about my daily care. All of my information, from all of my devices is uploaded to the same place where I can see it all and it was easy!
Will I need to change both of these devices to make life easier? What will the overall software platform be that I use?
I want to be able to upload/Bluetooth/cloud sync all my devices to the same place!
I want to use whatever d*** device I like best. And I really don't like that I have to research all of this when managing diabetes is enough work already.