In this post, I will provide a short summary of the information revealed from parliamentary question responses on how many people in Ireland use insulin pumps, what clinics provide them as a treatment option and how many new pump starts are done each year.
Making Sense of the Glycaemic Index
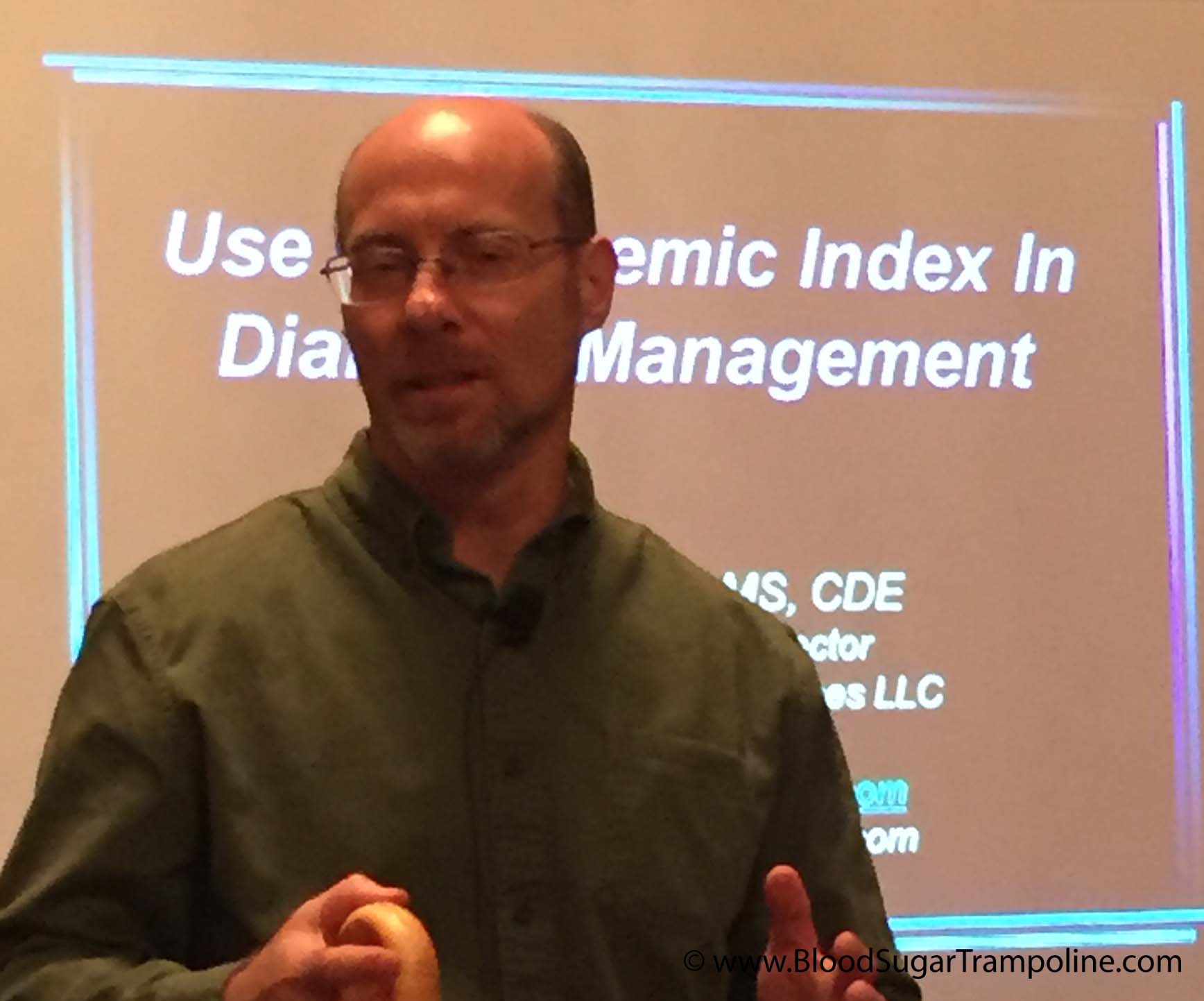
Mid October, I went to the DiabetesSisters Weekend for Women conference Alexandria, Virginia. See disclaimer at the end. One of the outstanding presentations I attended was by Thriveabetes 2016 speaker, Gary Scheiner’s presentation on “Making use of the Glycaemic Index”. This should not be a surprise to anyone has read Gary’s book “Think Like a Pancreas”. I will be honest here; when I heard the words “Glycaemic Index” I pretended I didn’t. And the reason is that several years ago, when it became a thing that was relevant to diabetes management, I tried to learn but I found it completely and utterly confusing. So I went to Gary’s talk as a skeptic.
BUT! As always Gary puts the information together well. See his blog posts here.
He started by saying that the glycemic index is the speed glucose enters the blood in the first two hours. It does not measure how fast foods enter the blood as glucose beyond that or how long it takes at all. A-ha! Ok so glycemic index is useful information for first two hours. I feel exonerated now.
This is hugely relevant to my diabetes management because I know that my rapid acting insulin peaks in approx 2 hours and that I might need additional insulin doses after that to cover the glucose released into my blood after the two hours.
The glycemic index is measured from 0 to 100. The closer to 100 a Food is, the higher its glycemic index is and the quicker the glucose hits your blood.
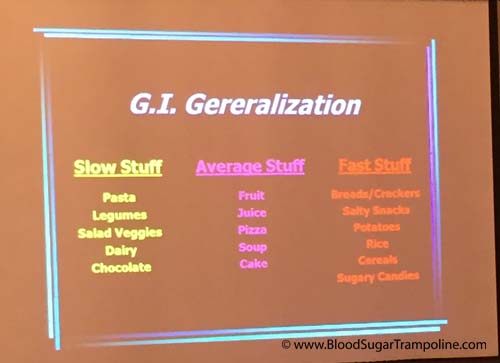
Here is a snapshot of the other things I learned;
- A mixed meal, ie a meal with protein, carbohydrates and or fat gravitates towards the carb. Meaning your body will process that first, albeit slower than if it was just carbs. So I might need to take a post meal dose of insulin in addition to my pre-meal dose.
- If you have a low GI food before your meal it will slow down the follow up starch in your meal. This is really good to know! Bring on the peanuts before the pasta or pizza :-)
- Larger portions take longer to digest. This isn’t new information to me but I suppose I always underestimate just how flippin’ long it takes.
- Time since your last meal affects the glycemic index. If you are still processing your food from the last meal, it’s going to slow down glucose absorption even more.

Some additional pieces of information not related to glycemic index but valuable.
- Don’t trust your CGM when you are recovering from a low. The lag time in full force.
- Insulin on board pump feature doesn’t take into account the food on board. As mentioned in the previous paragraph, if you are still digesting food you may need to override the insulin on board recommendation.
- Insulin resistance can happen if you have a meal with a lot of fat.
- Protein to insulin formula = ½ The total of protein grams and treat as carbs.
- Amylin/Symlin is a hormone that slows gastric emptying. People who don’t have insulin don’t have amylin either so stomachs process food quicker.
- Victoza is a GLP-1 injectable medication and reduces glucagon secretion; slows down the absorption of food.
In summary, glycemic index important to people with diabetes because:
- Satiety. Low glycemic index meals help you feel full for longer.
- Helps with the Timing of insulin. For example, if you know a meal or snack is going to have a high glycemic index then you could take your insulin 15 - 20. Minutes beforehand to give it a head start.
- Helps avoid post meal spikes
So, I’m glad that I learned all of this and I’m glad that I don’t have to waste any more of my time trying to figure it out because it makes more sense to me now. And It may help me to know the glycemic index of a Food I’ve never tried before so that I can figure how to deliver my insulin (pre-meal, at meal or extended Bolus).
Disclaimer: Diabetes Sisters paid for my conference registration and accommodation but also gave me a contribution towards my travel costs. All they asked for in return was that I would write a blog post about the conference which I had to do anyway because I learned so much that needs to be shared;-) And I wrote here about how I was selected.
Weather the diabetes havoc-er
One of the factors not included in Diatribe’s 22 factors that influence glucose levels is the weather. Sometimes the weather plays with my diabetes management. And here’s how. Do you remember that really, really wet day we had last week? It seems like a distant memory now and I don’t think it had a name, like a storm name, but most of the country was flooded under a yellow weather warning.
When I got up that morning and look out the window I thought “Nope, I’m not walking, I don’t mind being wet and drippy but not that wet!” I was disappointed because most days I love my walk. It clears my head as I inhale clean fresh energy and exhale stress. I swing my arms vigorously and loosen up my neck and shoulders. I had missed my walk the day before due to a doctor's appointment so I was doubly disappointed.
So, with my daily constitutional off the menu, I took my “no-walk” breakfast insulin dose, which tends to be twice what I take if I am walking and off I drove the kids to school.
However, as I was dropping the teen and preteen to school the rain wasn’t that bad. So,I changed my mind (GASP)…. but how can I avoid a hypo seeing as I’ve taking all this insulin without using calories to prevent the low glucose reaction that will surely follow?
I decided to turn my background/basal insulin down to zero for one hour on my insulin pump. Yes, it was going to take an hour to take effect but it was better than a severe hypo. At least it might soften the blow.
Now, if I was on injection pens there is no way I could have avoided preventing a low without glucose.
So was I successful? Weeelll, kind of. I did have a hypo. A doosy at 2.8mmols but it didn’t feel as bad as it was and I didn’t feel like I had to consume the entire kitchen just about a dozen small jellies.
Compared to most hypos this one rebounded quite quickly and not too high. However, I did spend most of the day with glucose levels that were more elevated than my usual.
And there you have it, diabetes the spontaneity killer and weather the diabetes havoc-er.
The Death of the Animas Insulin Pump
Last week, Johnson & Johnson Diabetes, who own Animas, announced that it was “exiting” out of the insulin pump business, effective immediately in the US and Canada. And eventually in the rest of the world. Once I read all the way down the press release to realise that it was just USA and Canada for now, I was relieved.
Then I was seriously miffed, but not completely surprised. Since the Vibe insulin pump was introduced, a number of years ago, innovation seemed to have stalled within the company. Johnson & Johnson own both Animas and the glucose meter company LifeScan/OneTouch but they didn’t even innovate between these products, not even to do what all others were doing and that was to sync products via Bluetooth or whatever internet cloud magic they choose. One might even say they really checked out of the diabetes industry a long time ago by their lack of interest.
So, what does this mean for us in Ireland? And what does this mean for me an Animas Pump user?
I have been using an Animas pump since my pumping beginnings in 2010. Then in 2014, I upgraded to the Vibe and in 2015 I added the Dexcom Continuous Glucose Monitoring System (CGM) to it. I didn't choose which insulin pump I would have, it was chosen for me, but I didn't have any complaints. In fact, it's been a great relationship!
Now I'm trying to think ahead and I realised that in the not too distant future I'm going to have to find a replacement for my insulin pump.
What are my choices in pumps? Do I actually have a choice, when the only other insulin pump my health service has a contract with is Medtronic? Yes it's probably a good pump but I don't want to be forced into it.
BUT it's not just my pump I need to consider!
This also effects my CGM device. How will my new pump interact with my current CGM, if at all? My Dexcom receiver IS my insulin pump, meaning that my glucose sensor transmits the information straight to my pump. So I need to either get a new receiver device or change CGM’s.
And then, there's my glucose meter which I was also able to upload to my insulin pump software programme which allows me to create useful graphs that help me make better decisions about my daily care. All of my information, from all of my devices is uploaded to the same place where I can see it all and it was easy!
Will I need to change both of these devices to make life easier? What will the overall software platform be that I use?
I want to be able to upload/Bluetooth/cloud sync all my devices to the same place!
I want to use whatever d*** device I like best. And I really don't like that I have to research all of this when managing diabetes is enough work already.
Thriveabetes; What is it? Why do I need it?
My children have been back to school for almost two full weeks now and since their first day back I've been spending a couple of hours most days planning Thriveabetes 2018. A month ago, at our fundraiser, I was asked to explain what Thriveabetes is, why people with diabetes need it and why I was asking people to give money to it.
After my nerve wrecking speech, several people commented on how they had no idea that living with diabetes was so involved and required so much work. Why I keep forgetting this when I talk about my diabetes I'll never know!
This post is to explain to people who don't have diabetes, what living with type 1 diabetes is actually like, to explain what our conference does for people with diabetes, why I'm passionate about it and why I need it.
Here's what I said;
What is Thriveabetes? And why do people with diabetes need it?
To answer these questions I have to, first, take you on a little journey. My journey.
I was diagnosed with type 1 diabetes 24 years ago as a young adult and It changed my entire life. I'd like to be able to say that living with type 1 becomes easier but it doesn't - it becomes habit.
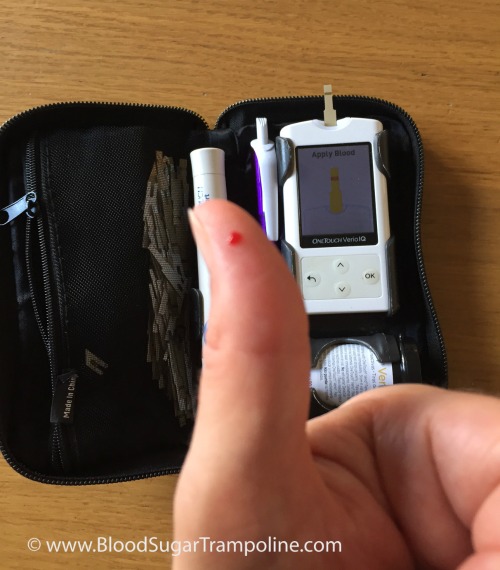
I woke up this morning, a little groggy because my glucose alarm went off during the night telling that my levels were a little high. So I got up, checked them on my meter, worked out a correction dose of insulin, took it and went back to sleep.
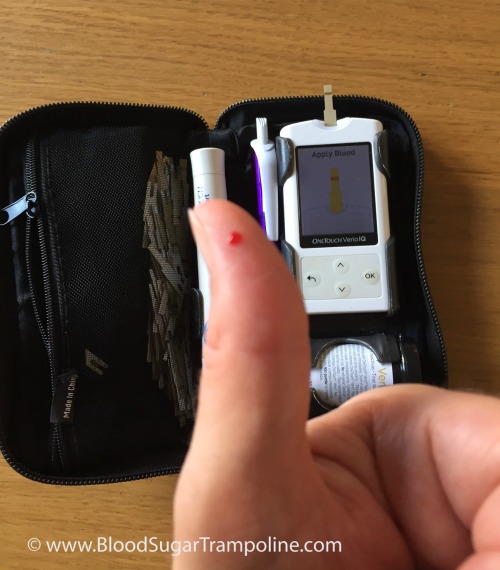 Before breakfast, I checked my levels again; they were in target, so I took my insulin for my regular weekend breakfast of tea and toast also known as 40g of carbs and then ate it.
Before breakfast, I checked my levels again; they were in target, so I took my insulin for my regular weekend breakfast of tea and toast also known as 40g of carbs and then ate it.
Two hours later with kids and car packed to travel across Ireland, I checked my levels again to see how close I came to getting it right. The answer was; not in target range, but close enough.
As I visited with my mother and family, I wondered what lunch was going to involve and when it was likely happen. It ended up being a sandwich at a Spar. I checked my glucose levels again. They were a little above my target, so I had to work out a correction dose of insulin plus working out an educated guess of how many grams of carbs were in this particular sandwich. Then I eat. My day, as with all other days, continued like this.
I do all of this out of habit. The numbers are very seldom perfect. But I get on with "close enough".
Now imagine, that the person with diabetes isn't you, but your child. So on top of all of those daily diabetes tasks that I do, you now have the added worry of “if I don't do this “close enough” my child is going to get sick. Again!”.
This kind of anxiety and stress goes on 24 hours a day, 7 days a week, etc. Diabetes NEVER takes time off. Ever.
This is why Thriveabetes is needed!
Thriveabetes is a place where you can relieve some of that stress and anxiety. The power and comfort of being in a room with so many people with diabetes, learning so much about managing daily life with it and knowing that every single person in that room knows diabetes like I do, lightens that load. There is no other place where we can get that.
It's a day that is organised completely by us; people with type 1 diabetes. We are all volunteers who are dedicated to and passionate about bring people with type 1 diabetes together to share what we deal with every day and to learn from world class speakers.
And that is Thriveabetes. And that is why I need it!
Blood Glucose Darkness
I've been using a continuous glucose monitor (CGM) since November 2015 and it has made a huge difference in my diabetes management. It has narrowed the glucose swings so much and it has been a huge relief in my anxiety relating to trying to avoid hypos. And I have worn it 24/7 since I got it. Last Friday, I had an MRI on my stupid 83 year old hip (another story) and I had to take my sensor off. So I decided to go the whole weekend cgm-free. I thought it would be nice to have a break from the alarms and just see how I got on.
I felt completely blind! I had no idea what my glucose levels were between finger prick checking and it was a huge loss of information. I felt I was making decisions with my insulin without all of the information.
That evening, I went to bed with a respectable glucose 8.8 mmols/L to be woken at 3am by perspiration steaming off my body of a glucose level of 2.8 mmol/L. I tried not to consume the entire kitchen and lay across the couch willing cold air to descend on me and cool me down.
Twenty minutes later, with glucose levels at 4.8 mmols/L and probably shooting for the sky in a rebound high, I had recovered enough to go back to bed. I woke with a glucose level of 11.5 mmols/L which was lower than I expected but still too high. At least, I was spared the high alarm during the rest of the night.
I can't believe that I used to think that I was doing fine on the information provided by 7 finger prick glucose checks per day! Using a cgm has taught me so much about how to manage my diabetes, it has taught me about creating more effective insulin doses and it has given me more power over my life with type 1 diabetes.
This piece of technology is really valuable for people with type 1 diabetes. However, I do realise that it isn't something that everybody would want or can get. I believe that availability will change in the near future though as more and more health care professionals realise its value in providing information beyond HbA1c’s also.