This week I’m taking part in the 7th annual Diabetes Blog Week, which runs from 16th to 20th May. Founded by Karen at Bitter Sweet Diabetes. Today's topic is The Other Half of Diabetes and I asked my other half, Mr. Blood Sugar Trampoline, who goes by the name of Phil, if he wanted to write something. I'm so thrilled he accepted. And speechless because.... well read for yourself.
The short version:
I've learned that we cannot control my wife's diabetes any more than we can control world hunger, but by taking a proactive role towards improving the healthcare environment and by supporting her empowerment, my anxiety over her health is not much different than my anxiety over my own health...and we're stronger as a couple because of her diabetes.
The longer version:
Next week, Gráinne and I celebrate our fifteenth anniversary of married life together. It has been a richly rewarding journey so far, and I look forward to continuing the journey for many many more years to come. I met her a few years previous, playing together on a softball team. I can't say as to when exactly I became aware she had type 1 diabetes; what I do remember is that as I began to learn her management regime, it seemed to my science-trained brain to be something fairly anachronistic...not that I really knew anything about medical best-practices for managing diabetes.
Back when I was 12 or so (in mid-80s USA), a boy in the grade behind me developed type 1 diabetes. All the more we were told was that he was sick, he's better, but he can't eat any sugar. "Here, try one of these diabetic candies!" Yuck. A decade later, I discovered a colleague had type 1 diabetes, she gave me a short primer that basically involved "testing blood sugar" and "injecting insulin." But I was otherwise ignorant.
It turns out, Gráinne didn't really seem to know a whole lot more than me - she knew there was an HbA1C number, along with her periodic blood sugar measurements, that were supposed to be "good" but was quite difficult to hit. And she knew that she needed to somehow adjust her insulin dose to her current blood sugar readings. She certainly didn't know much (if anything) about carb counting. As to what causes diabetes, how it affects the body, how behaviour and diet interact...these were all things that she wasn't learning from her doctor.
So I asked her "where can I learn more about this?" And I asked myself "how do we fix it?"
I suspect my reaction to diabetes is similar to PWD who are scientifically-minded and wanting to get on top of this thing...only I have the luxury of not having the terror that is "I am going to lose my vision and my limbs and die in childbirth." (I failed to mention that as part of my diabetes education, I had seen Steel Magnolias, which frankly could be an entirely separate blog post.)
Certainly, there are echoes of my thinking in how a college roommate (and fellow physics major) took on his wife's type 1 diagnosis in her late 20's. "This is surely just a simple function of carbohydrate, metabolism, insulin, and time that results in a blood glucose reading of X..."
As I am sure many of you were shocked to find out, it turns out it's not quite so simple. Fats, the kinds of sugar (including alcohol), fibre, hormones (stress and otherwise), circadian rhythms, fatigue...and other variables like insulin that can go off, injection site, temperature. OMG this thing is so damn FRUSTRATING. And it's not even my body it's happening to.
About a year after getting married, we moved to Minneapolis for a few years of "getting to know my people." We took advantage of the healthcare system there - my former colleague gave us a brilliant referral to a team of diabetes care professionals who really helped Gráinne learn some better tools and techniques for managing her diabetes. For me, the most important outcome of this was that Gráinne started to become empowered in her own management.
When we moved back to Ireland, it was as if we stepped back in time. There was no medical team looking after body and soul...just arrogant doctors who got upset when you didn't do everything you told them (eating the same food every day? Seriously?). It didn't seem that Irish doctors really understood the fact that diabetes is not a simple equation. She has changed doctors way more frequently than is the norm in Ireland, seeking to find a fit as good as what she found in Minneapolis.
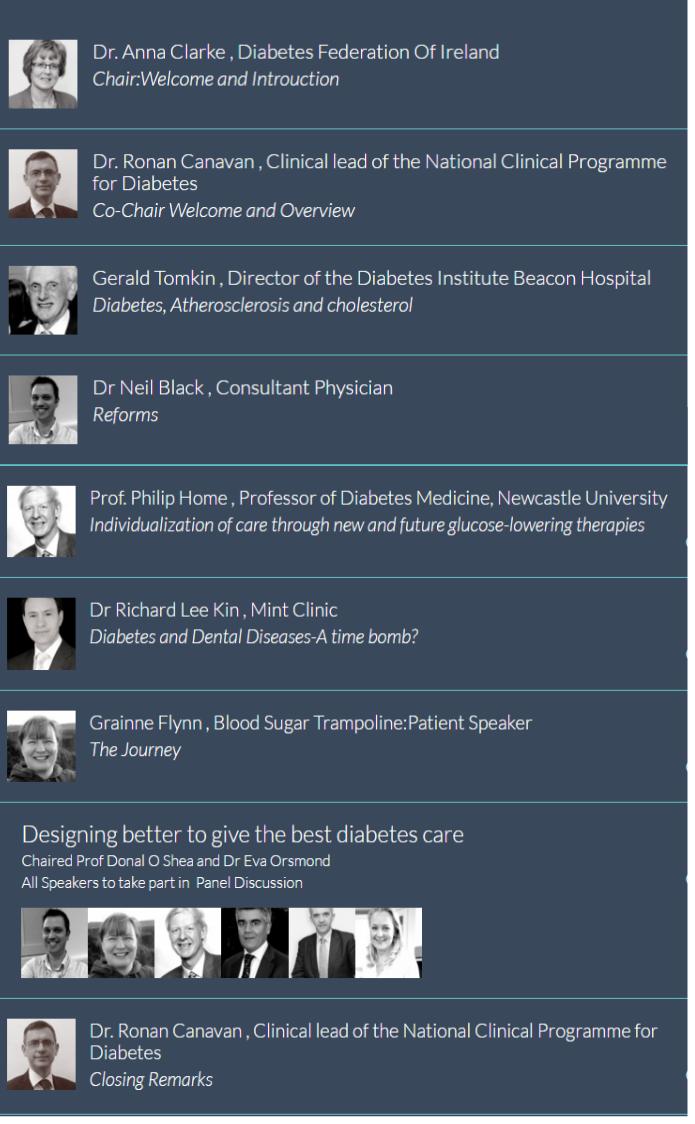
So, in addition to shaping Gráinne's personal environment, we set out to improve the environment for everybody in Ireland. We did this by getting involved with Diabetes Ireland (then called the Diabetes Federation of Ireland). You learn a lot when you get out of a "selfish" mode of working - perspective builds empathy. Community is empowering - there is great power in numbers. When these numbers are singing in concert while they're rowing in one direction, bureaucratic and institutional inertia can shift.
As a person I love deeply, I of course worry about Gráinne's physical health. Her diabetes doesn't weigh on my mind anywhere near as much as it does on hers, but it's there. Hypos scare me too (and selfishly, I'm glad Gráinne found that a CGM suits her...nighttime hypos she slept through are scary on a whole other level).
But being totally honest here, the thing I worry far more than her physical health is her mental health. If Gráinne is stressed, that stress will invariably become my stress, and our family's stress. If this stress were chronic, life would be pretty damn miserable for all of us. Chronic health conditions can wear you out. Ask anybody with Lyme disease, MS, Crohn's, HIV, chronic migraines, or frankly any other chronic condition. But in some ways, type 1 diabetes is different.
Type 1 asks its patients to undertake medical decisions multiple times per day, without consulting a medical professional, using nothing more than education and wits. If you make the wrong decision you could end up in a coma or dead. Or, if you make less-wrong decisions but do that a lot over time, you could end up blind or limbless. And then there's the possibility of making the "right" decisions (i.e. one the medical professional would suggest), all of this bad stuff could happen to you anyhow.
What can I do to keep her head healthy? I try to make sure she knows she's supported, and I try to "nudge" her in the direction she's looking but hesitating to head. (As her confidence has built, there's been much less nudging.) Sure there are down times, frustrating times. She sometimes needs to vent, I can do nothing but sit there and listen, and give her a hug.
But that's not "diabetes life," that's "life life." It just so happens we have this extra topic of stress and frustration that most other married couples don't have. But we also have this extra source from which to build strength.
When we said our marriage vows fifteen years ago, we already knew some of the "sickness" part. We've been incredibly fortunate to be able to leverage that sickness into a source of strength and bonding. If I could cure her diabetes, I would in an instant...but in some strange way I don't think I could imagine life without it.
Phil & I don't really talk about diabetes much, I suppose after 15+ years of being together there are somethings that you don't have to say but sometimes we might forget. Thank you Phil and here's to another fun-filled 15 years.







 I’m sooooooooooooooooooo excited about taking part in my very first
I’m sooooooooooooooooooo excited about taking part in my very first 

 However, I hear a lot of talk about ketones and began to think that, maybe, I'm a bit too relaxed about them and need to know a bit more.
However, I hear a lot of talk about ketones and began to think that, maybe, I'm a bit too relaxed about them and need to know a bit more.