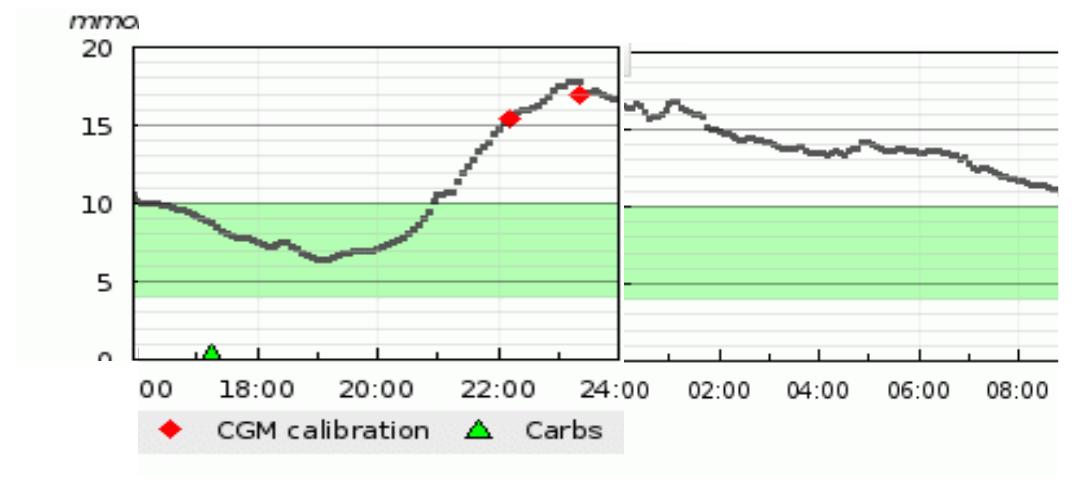
The HSE approved funding for my Dexcom G4 continuous glucose system since November (love it!); I received my start up kit through funding from HSE’s community care budget.
My Animas rep called me in January to tell me that my Dexcom G4 Platinum Sensors had been, finally, approved funding for them through Long Term Illness scheme. All I had to do was get my GP or consultant to update my long term illness book and bring it to my chemist.
In the meantime, she rang my chemist to explain that all that needed to be done was underway and gave them all the information they needed to order my sensors. Yay!

As I wasn’t due to meet my consultant until April (approximately) I decided to go my GP. I had everything I needed in hand. I knew exactly what I had to ask for. What could go wrong?
LORD ABOVE, GIVE ME STRENGTH TO DEAL WITH OTHER PEOPLE’S BAD DAYS.
After waiting one hour to be seen by my gp I left within 10 minutes, without what I needed. I met with the most “by-the-book” (yeah like anything about diabetes is by the book) and “professional”(not) GP, who by the way assured my on next visit that he WAS quite popular!
What happened?
Well, this chap, who is filling in for my regular gp, decided to focus on semantics. My LTI book had not been updated for 6 years, which is kind of a technicality but kind of not. He questioned me like an FBI agent about every item he had to list. He was very concerned about if I needed it every month or not??? It didn’t actually matter?!? But I didn’t know that yet.
I had to explain why things like a Hypo emergency kit, or Novorapid flex pens, needed to be included on my script for emergency situations.
All of a sudden, he threw his pen down and said I really don’t know what I’m doing here, can you go to your chemist and get a list of all your meds? Even though, it was right there in front of him! He added something to the effect of diabetics come in here asking for all this stuff that I don’t know about. (?!?!?!).
It was clear to me that he was done with me. And I was done with him. I was having a difficult time remaining calm and trying to figure out what to do.
I left in a state and decided to go direct to the source of all information required.
He gave me the impression that his problem was he didn’t know how to fill out my prescription as required by the long term illness scheme. So! I hopped into my car and drove over the Long Term Illness Section in Ennis.
I explained what had just transpired and asked for a guide for snotty GP’s on how to fill out prescriptions for the LTI scheme. The lady was really nice and explained everything. But I then had to remember it!
What I learned in the Long Term Illness Dept that I did not already know.
She told me the following;
- My GP should always have an updated list of all the medicines I use - regardless of who writes the prescription. My consultant should be writing to him with this information. (Does that actually happen? I know this wouldn’t be high on my priority list.)
- The LTI book does not need to be updated every six months. (The book itself says it does, the chemist says it does; I’m going with “it does”.) However, updated does not mean submitting it to LTI every six months. It means that the GP/Consultant writes out the prescription in the space (the yellow pages) provided every 6 months and you bring it to your chemist.
- If the item being prescribed is on the HSE’s List of approved medical supplies for diabetes known as “Core List F”, my GP only needs to write what the item is, he does not need to write a quantity. Once the item is on this list it is approved. So, again, no need to submit to LTI just take it straight to the chemist.
- However, if the item is not on Core List F but is on the “Special Product List”, then a quantity may be required.
If the item you are after is not on either of those lists this page might help you.
Ok! Onwards! I went home. All the while I practised deep breathing. As soon as I got home I called the GP office and rescheduled my appointment (another reason to be p****d off).
Next day, I arrive to his office to receive a “what can I do for you today?”(?!?!?!). At this point, I found it more than very difficult to stay close to calm and civil, while explaining why I was offended, frustrated with him, and annoyed.
All of which was news to him! He even had the naivety to tell me this was the first time someone has a problem with his bedside manner and that he was actually quite popular in the practice. I knew I couldn’t tell him he sounded like a twenty year old creating his first CV because I wasn't trying to offend him like he did to me.
I never heard the words “sorry” or “apologise” during our 15 minute consultation. No stepping down off the deity pedestal AT. ALL.
And so, I won’t be going back to him and I know it’s no skin off his nose. He can continue to be arrogant and emotionally immature….. until it bites him in the ass:-)
Because you know what goes around comes around - always.






 Good diabetes management is possible while using multiple daily injections. An insulin pump won't magically fix most of your problems with your diabetes - they are a lot of work. So if you are interested in moving to a pump, do your homework and find out exactly how you might benefit, google them, read book on them, talk to one of the representatives from the 2-3 companies who provide pumps in Ireland, talk to other people who have used them, and talk to people who tried them and it didn't work.
Good diabetes management is possible while using multiple daily injections. An insulin pump won't magically fix most of your problems with your diabetes - they are a lot of work. So if you are interested in moving to a pump, do your homework and find out exactly how you might benefit, google them, read book on them, talk to one of the representatives from the 2-3 companies who provide pumps in Ireland, talk to other people who have used them, and talk to people who tried them and it didn't work.