Navigating your diabetes clinic can be so confusing. This is a guide to the who’s who in your diabetes healthcare team which is extremely useful because it can save so much time and frustration during your appointments, when you direct your questions to the appropriate person.
Making Sense of the Glycaemic Index
Mid October, I went to the DiabetesSisters Weekend for Women conference Alexandria, Virginia. See disclaimer at the end. One of the outstanding presentations I attended was by Thriveabetes 2016 speaker, Gary Scheiner’s presentation on “Making use of the Glycaemic Index”. This should not be a surprise to anyone has read Gary’s book “Think Like a Pancreas”. I will be honest here; when I heard the words “Glycaemic Index” I pretended I didn’t. And the reason is that several years ago, when it became a thing that was relevant to diabetes management, I tried to learn but I found it completely and utterly confusing. So I went to Gary’s talk as a skeptic.
BUT! As always Gary puts the information together well. See his blog posts here.
He started by saying that the glycemic index is the speed glucose enters the blood in the first two hours. It does not measure how fast foods enter the blood as glucose beyond that or how long it takes at all. A-ha! Ok so glycemic index is useful information for first two hours. I feel exonerated now.
This is hugely relevant to my diabetes management because I know that my rapid acting insulin peaks in approx 2 hours and that I might need additional insulin doses after that to cover the glucose released into my blood after the two hours.
The glycemic index is measured from 0 to 100. The closer to 100 a Food is, the higher its glycemic index is and the quicker the glucose hits your blood.
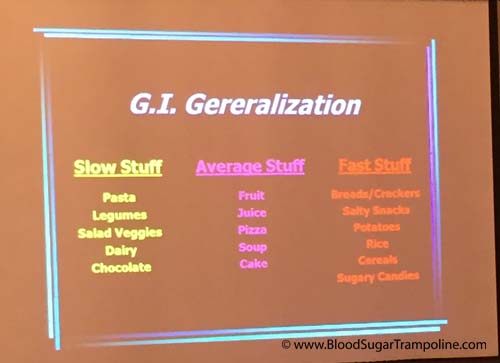
Here is a snapshot of the other things I learned;
- A mixed meal, ie a meal with protein, carbohydrates and or fat gravitates towards the carb. Meaning your body will process that first, albeit slower than if it was just carbs. So I might need to take a post meal dose of insulin in addition to my pre-meal dose.
- If you have a low GI food before your meal it will slow down the follow up starch in your meal. This is really good to know! Bring on the peanuts before the pasta or pizza :-)
- Larger portions take longer to digest. This isn’t new information to me but I suppose I always underestimate just how flippin’ long it takes.
- Time since your last meal affects the glycemic index. If you are still processing your food from the last meal, it’s going to slow down glucose absorption even more.

Some additional pieces of information not related to glycemic index but valuable.
- Don’t trust your CGM when you are recovering from a low. The lag time in full force.
- Insulin on board pump feature doesn’t take into account the food on board. As mentioned in the previous paragraph, if you are still digesting food you may need to override the insulin on board recommendation.
- Insulin resistance can happen if you have a meal with a lot of fat.
- Protein to insulin formula = ½ The total of protein grams and treat as carbs.
- Amylin/Symlin is a hormone that slows gastric emptying. People who don’t have insulin don’t have amylin either so stomachs process food quicker.
- Victoza is a GLP-1 injectable medication and reduces glucagon secretion; slows down the absorption of food.
In summary, glycemic index important to people with diabetes because:
- Satiety. Low glycemic index meals help you feel full for longer.
- Helps with the Timing of insulin. For example, if you know a meal or snack is going to have a high glycemic index then you could take your insulin 15 - 20. Minutes beforehand to give it a head start.
- Helps avoid post meal spikes
So, I’m glad that I learned all of this and I’m glad that I don’t have to waste any more of my time trying to figure it out because it makes more sense to me now. And It may help me to know the glycemic index of a Food I’ve never tried before so that I can figure how to deliver my insulin (pre-meal, at meal or extended Bolus).
Disclaimer: Diabetes Sisters paid for my conference registration and accommodation but also gave me a contribution towards my travel costs. All they asked for in return was that I would write a blog post about the conference which I had to do anyway because I learned so much that needs to be shared;-) And I wrote here about how I was selected.
Diabetes on steroids
Back in October, I had a steroid injection in my hip. And yes, it drove my glucose levels bananas! For those of you who may not be aware of it, steroids are one of the medications that truly mess up glucose numbers for lots and lots of people. The ultimate craziness only lasted two to three days but the residual crazy lingered a couple of weeks.
Here’s a little of the backstory behind why I got a steroid injection.
I have been complaining about my right hip for some time and I finally did something about it in September 2016. I went to my GP. He referred me to my physiotherapist and we did some “process of elimination” exercises. They didn't work. So then I went for an MRI and was referred to a rheumatologist.
At least now, we think I know what is wrong with my hip! It would seem both my physiotherapist and my rheumatologist agree that I have bursitis. And my rheumatologist injected steroids to reduce the swelling. If you have diabetes and you have steroids that plays absolute havoc with blood glucose.
However, no one could tell me how many days, weeks, months the glucose madness would go on for and how severe it would be.
Here is my experience of what happened to my glucose levels.
Prior to my injection my diabetes management was going fairly well with just the usual ups and downs. I had the shot mid morning and my glucose levels didn’t feel the effect of the injection until after lunch. But after lunch my numbers remained in the high teens until the early hours of the next morning. On day two, I noticed that if I increase my mealtime insulin significantly more than usual it would keep them in check. However, if I forgot to make the increase then I struggled to bring my numbers back down for hours.
Then the effect of the steroid started to wane slowly over the next two weeks and I had the opposite problem: trying to keep my glucose levels above hypo level. I adjusted insulin doses slowly and only making one or two changes at a time to bring them back to my normal diabetes levels (?!?!).
I was grateful that not only was I aware that this would more than likely happen but that both my endocrinologist, rheumatologist and physiotherapist reminded me it would. I'm probably going to have another dose in January but now, at least, I have a good idea of what to expect.
Social Media & Information Blindness
I'm beginning to feel like I am becoming blind to information if it's not being blasted at me on social media. If it's not a flashy click bait image. And I think it's making my brain die slowly.

Last week, my husband told me, (and I heard him tell me!!!, not the nod and yes response), that our broccoli in the garden was ready for picking and we shouldn't buy any for a number of weeks. Shortly after being told this, like an hour, I was doing the shopping and saw that broccoli was half price. What a bargain, I thought and bought it. What happened to my brain? Where did that piece of information go??
Is it that I'm so used to having instant information and that information is so easy to retrieve at any time on any device that my brain has forgotten how to retain information?
Ireland in the 80's it was so easy to inform people and be informed. We only had two tv channels (rural Ireland that is - No Sky channel for us), two national radio stations and maybe one weekly local newspaper, we did have a couple of daily national broadsheets too. this meant was it was extremely difficult to be unaware of anything newsworthy and if you needed to get a public information message to the people the telly and radio were both sure things.
These days though it’s extremely difficult to reach out to people with information. Unless, of course, you spend a large fortune in advertising and then there are still people who are unreachable.
When something changes in the diabetes health service how do we let people know?
In the last few years there have been at least three major changes that affect people with diabetes in Ireland. This is just off the top of my head.
- In 2014, the HSE rule which prevented people with diabetes from holding both a medical card and a Long Term Illness book was changed to allow it. This meant that thousands of people with diabetes had to be informed that they now needed to apply for the LTI and should not be paying a prescription charge for the diabetes supplies and medications. I’m still coming across people in the diabetes online community who haven’t been informed of this!!!
- In April 2016, Restrictions were placed on blood glucose meter test strips for people who do NOT use insulin. See here.
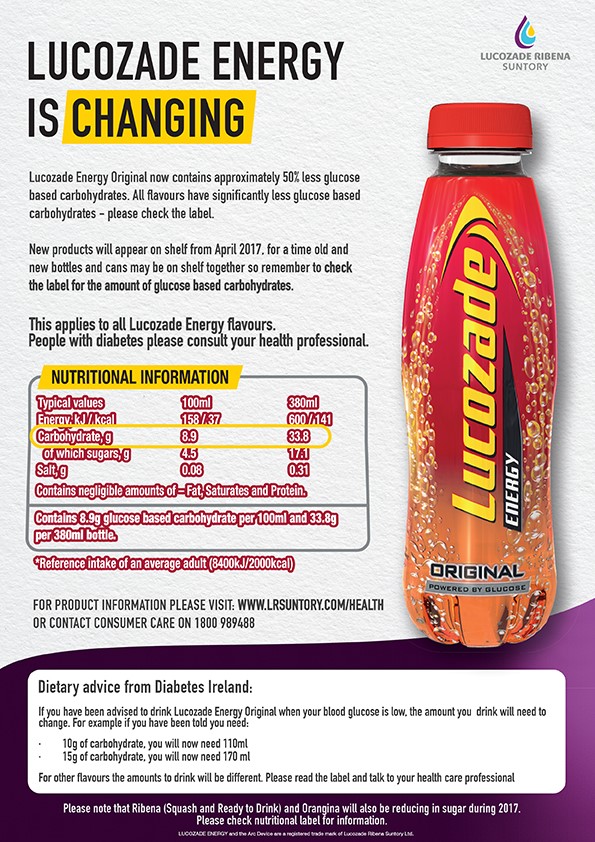
- Most recently, April 2017, the change in the sugar content of Lucozade in both UK and Ireland. Every diabetes organisation and group carried this news and it even made it into mainstream media in both countries. There were posters in diabetes clinics (however, we are all looking down at our phones) all over the country. And there are still people who have not received this information, even though they are actively engaging in social media for their diabetes information. There are also people living in this world who even if you put the information right under their noses they still won't see it. And given my broccoli evidence above this could be me!?! Aaaahhh!
This makes me hugely worried for the all of those people with diabetes who do not engage online for diabetes information. We tend to forget that a very large portion of the diabetes community is not engaged online at all. We can't rely on the diabetes medical teams to reach every single person who attends their clinics with new information - it's just not feasible or even possible. Someone will always slip through.
I think this is why offline diabetes peer support can play a huge role. We can help make sure noone falls through!
Empowerment and Diabetes - My Journey
Last May, I was asked by the organisers of the Future Health Summit to give a presentation on how I became an empowered person with diabetes. Some friends asked if I could blog about it. The reason for my topic choice was because the theme of the conference was Empowering the Patient, Information, Choice & Accountability and I decided to focus on Empowering the Patient element for my presentation. I feel like I am one, that diabetes does not have power over me, I have a lot of power over it.
The journey towards being an empowered patient didn’t happen overnight, for me. I would like to think that a person with diabetes diagnosed today would find empowerment much quicker than I did. But the two core elements that were pivotal in my journey didn’t really exist when I was diagnosed. Those elements were Diabetes Education & Support.
Obviously my Journey Began with diagnosis 23 years ago - 1993. Diabetes Education was extremely basic in Ireland back then, if it existed at all!
My diabetes management involved;
Injecting a fixed amount of insulin twice every day
Eating the same amount of food at the same time every day
Checking Blood Glucose levels just twice every day
And I was taught How to recognise & treat a hypo
For those first 6 years I felt like I blindly coasted through my diabetes care. I did what I was asked to but I had no idea why I was doing any of it, except to stay alive.
So what changed? What prompted me to get on the bus to empowerment?
This is going to sound corny but it was love. In 1999, I met this bloke.
Phil
This is Phil. We weren’t going out very long but he already had notions about our relationship and we weren’t going out for very long when he asked me for books or leaflets where he could learn more about helping me manage my diabetes. I was stunned! And for three reasons;
He was the first person I met who didn’t expect me to educate him on something I barely knew myself.
That the relationship was moving a bit faster than I had thought and
that I had nothing, absolutely nothing to give him when it came to information.
What I did have was access to the internet at work. So the next day, during my lunch break, I “AltaVista’d” type 1 diabetes. If you don’t know what AltaVista is, google it! :-D
I couldn’t believe what I found - the list of websites containing information was so long. I found all of these organisations with websites that had tonnes of practical information such as the Joslin Diabetes Centre and the world’s leading research organisation, the JRDF. I had never heard of these places before.
I started reading all of this information before handing it over to Phil and it got me thinking that there might be a better way to live with diabetes. But that thinking got shelved for a while as this journey is not an express route and it required a couple of transfers to reach my destination.
1st Transfer–Diabetes Education
You’ll be happy to know that I, very quickly, realised Phil was a keeper and by 2003, we had been married a couple of years, had moved to US and we were thinking about starting a family. As soon as my endocrinologist heard this he marched me off to a dietitian to learn about counting carbohydrates, insulin dose adjustment and sliding scales.
I had been diagnosed 10 years by the time I found diabetes education which now seems too long. But this knowledge gave me some of the control over this thing called diabetes for the first time. And I felt supported; supported by my diabetes team and supported with knowledge. I didn’t realised it then but my diabetes team in the US was the first I experience of patient centred care.
Family 1
family 2
2nd Transfer–Diabetes Peer Support
The 2nd transfer on my journey towards empowerment was finding peer support.
By 2007, we had moved back to Ireland, had our second baby and I was increasingly frustrated and unhappy with the diabetes care I was receiving. In June of that year I found myself at my lowest point after leaving the most humiliating diabetes appointment I’ve ever experienced. But it propelled me into action. I knew there had to be someone out there who would make me feel listened to.
I went home and remembered a recent newspaper article about a new branch of Diabetes Ireland being set up in Clare. I called the number in the piece and the lady who answered was a fellow person with type 1 diabetes. What are the odds? She had had her second baby around the same time as I had and we were both new to Clare. We instantly connected and during the course of that conversation we realised that we both wanted to meet more people like us and to do this was to set up diabetes support groups.
By the end of 2007, we had diabetes support groups and they continue to be a source of information, motivation and inspiration for me. And they, with some information from Diabetes Ireland helped me find a diabetes team that works amazing for me.
support group
Destination Reached - Person Empowered
This is where I feel my journey towards empowerment was completed. I had reached my destination.
Yes, I took the scenic route to being an empowered person with diabetes. An empowered person with diabetes who can drive her own diabetes. And I became that by finding two very simple, very basic diabetes resources but yet they are not accessible to everyone with diabetes in Ireland.
The first necessity is Diabetes education is as important as giving someone who wants to drive a car lesson and some theory. Would you really put a beginner in the driving seat of a car without it? And not just structured diabetes Education, like the university style of lectures. This education has to be an ongoing 2-way conversational style of learning, where a person with diabetes can grow in confidence, drive their own diabetes and the instructor takes more of a back seat each time.
The second is Diabetes Support and for me that comes from three sources;
At home - I may be the person with diabetes but my whole family lives with it. The more supported I am at home the more successful I will be in my diabetes management.
My Diabetes team - My journey has taught me that I need a health care team who listens to me, acknowledges all that I do to manage my care and doesn’t just focus my failings. A team that continues to teach me and a team that continues to learn.
My diabetes Peers – the most undervalued, underused resource available for people with diabetes today. Who else knows what it’s like to live with diabetes than other people with it. We learn so much from sharing our experiences, so much that can’t be taught in a hospital appointment.
So while my journey towards empowerment has been completed, my life with diabetes journey still continues. And I hope to continue that journey for many, many decades.
What is Diabetes
Chances are that if you found my website you already know a little something about diabetes. But, you might be like me and always want to learn more. And there's ALWAYS is more to learn about diabetes. In this page/post I will attempt to give you my interpretation of diabetes. But I will also refer to medical people who can get more technical. I will also talk about the symptoms of diabetes, the risk factors and different types of diabetes. Diabetes is not easy to explain and it usually requires more than a short sentence, which means people's eyes glaze over and you lose them before you get to the "good" stuff. But you still have to try right.
It's important for all of us, people with diabetes, to not only explain our type correctly but when we are asked about other types that we support those people well too.
Let's start with the basics. Most of the medical definitions I've used here came from the Canadian Diabetes Association's website.
Diabetes is;
Diabetes is a lifelong, chronic, and sometimes fatal disease about the struggle to manage glucose levels in your bloodstream. The body either cannot produce insulin or cannot properly use the insulin it produces.
What do we need insulin?
Insulin is a hormone that turns the glucose (sugar) in our blood into energy for all of our cells to function. The glucose comes from a couple of sources, mostly from foods known as carbohydrates and a stored supply in our liver. Diabetes leads to high blood sugar levels, which can damage organs, blood vessels and nerves - every where our blood goes means that's an area excess sugar can damage. - See more here.
There are a bunch of different types of diabetes.
Type 1 Diabetes
My (non scientific, non-medical) description; Type 1 diabetes happens when, for some unknown reason, our immune system goes "terminator" on our insulin making cells and wipes them all out. My body now has no way to convert the food I eat, in particular the good stuff that comes in the form of carbohydrates, into fuel for my body to exist. Or the glucose that is constantly being released from my liver to keep energy levels up in between meals.
About five to 10% of people with diabetes have type 1 diabetes and it can happen at any age. Type 1 diabetes generally develops in childhood or adolescence, but can develop in adulthood. And type 1 diabetes is always treated with insulin."
For the more medical explanation of type 1 diabetes click here. "The risk factors for type 1 diabetes are still being researched. However, having a family member with type 1 diabetes slightly increases the risk of developing the disease. Environmental factors and exposure to some viral infections have also been linked to the risk of developing type 1 diabetes." Source - International Diabetes Federation (IDF)
Symptoms of Type 1 Diabetes:
The symptoms of type 1 diabetes can develop very quickly (over a few days or weeks), particularly in children.
The main symptoms of type 1 diabetes are the 4T's :
- Excessive Thirst
- Excessive trips to the Toilet
- Excessive Tiredness
- Thin; losing an excessive amount of weight
Other symptoms can be vomiting or heavy, deep breathing can also occur at a later stage. This is a dangerous sign and requires immediate admission to hospital for treatment. For more information on the symptoms of type 1 diabetes, click here.
LADA (latent autoimmune diabetes in adults) or Type 1.5
My (non scientific, non-medical) description; LADA is very much like type 1 diabetes but it tends to occur in older adults. It is very often mistaken for type 2 diabetes. It's a slower destruction of the insulin making cells. Maybe it's something to do with the "Terminator" being older and slower moving!?! So the symptoms present over a longer period than they would for a person with type 1 diabetes.
LADA is also known as slow-onset type 1 diabetes and type 1.5 diabetes. Like other forms of type 1 diabetes, people with LADA require insulin injections to normalise their blood glucose levels.
For the more medical explanation of LADA click here. Symptoms are very similar to those of type 1 diabetes.
Type 2 Diabetes
My (non scientific, non-medical) description; Type 2 diabetes happens when your insulin has developed a dementia. It's old and tired and not quite sure what it's suppose to do. So, sometimes it works and sometimes it has to put twice as much effort in to work. To me, it's like the insulin has dementia - sometimes it's sharp and works well and other times it just can't figure out what to do.
In general, people who develop type 2 diabetes are older but this isn't always the case. it's the most common type of diabetes.
The treatment options for type 2 diabetes include managing physical activity and meal planning, or may also require medications and/or insulin to control blood sugar more effectively. It can be a series of trial and error to find the right treatment plan for a person with type 2 diabetes.
For the more medical explanation of type 2 diabetes click here.
Symptoms of Type 2 Diabetes:
The symptoms of type 2 diabetes can be very slow to present and often you can have type 2 diabetes for a number of years before it is picked up.
The most common symptoms of type 2 diabetes include:
- excessive thirst
- frequent or increased urination, especially at night
- excessive hunger
- fatigue
- blurry vision
- sores or cuts that won’t heal
Risk Factors for Type 2 Diabetes (from IDF):
There are 10, that's TEN risk factors for type 2 diabetes. Not just the two/three that we ALWAYS hear about.
- Family history of diabetes
- Increasing age
- High blood pressure
- Ethnicity
- Impaired glucose tolerance (IGT)*
- Overweight
- Unhealthy diet
- Physical inactivity
- History of gestational diabetes
- Poor nutrition during pregnancy
Impaired glucose tolerance (IGT) is a category of higher than normal blood glucose, but below the threshold for diagnosing diabetes.
Gestational Diabetes
The other description from IDF; is a form of diabetes consisting of high blood glucose levels during pregnancy. It develops in one in 25 pregnancies worldwide and is associated with complications to both mother and baby. GDM usually disappears after pregnancy but women with GDM and their children are at an increased risk of developing type 2 diabetes later in life.
Approximately half of women with a history of GDM go on to develop type 2 diabetes within five to ten years after delivery.
Other Types.
There are other, much rarer forms of diabetes that are monogenic, meaning a change in only one gene is responsible for the condition. There are two types of conditions in this category: Maturity Onset Diabetes of the Young (MODY) and Neonatal Diabetes Mellitus (NDM).
For these types of diabetes I have to call on the words of experts because I'm not very familiar with them and don't feel comfortable giving a description of something I don't know much about.
MODY Maturity Onset Diabetes of the Young
I would love to take credit for this explanation of MODY but I couldn't do any better than Morag (Twitter: @SparklyRedShoes) on GBDOC ; MODY happens when there is a mutation of a gene and is most often hereditary. It very often is confused as type 2 diabetes in a young person.
"MODY is diagnosed by genetic testing. It may be worth testing for MODY when a person with diabetes doesn’t fit the profile of the more usual types. For example, somebody who actually has MODY may not require as much insulin as most people with Type 1 (and will have measurable C-peptide), even long after the honeymoon period, but they will generally not be of the age and weight you might expect to see for Type 2. In fact, at diagnosis, people with MODY are often young, slim and active. "
Being genetic, it runs strongly in families; if one parent has it, then the chances of a child inheriting the gene are 50/50. People with a MODY gene generally develop diabetes as young adults, and most are diagnosed by age 45.
For the more medical explanation of type 2 diabetes click here.
The key features of MODY are;
- Being diagnosed with diabetes under the age of 25.
- Having a parent with diabetes, with diabetes in two or more generations.
- Not necessarily needing insulin.
NDM Neonatal Diabetes Mellitus
 From Diabetes UK; Neonatal diabetes is a form of diabetes that is diagnosed under the age of nine months. It’s a different type of diabetes than the more common Type 1 diabetes as it’s not an autoimmune condition (where the body has destroyed its insulin producing cells). Like MODY it's a genetic mutation.
From Diabetes UK; Neonatal diabetes is a form of diabetes that is diagnosed under the age of nine months. It’s a different type of diabetes than the more common Type 1 diabetes as it’s not an autoimmune condition (where the body has destroyed its insulin producing cells). Like MODY it's a genetic mutation.
The key features of neonatal diabetes are:
- Neonatal diabetes is caused by a change in a gene which affects insulin production. This means that levels of blood glucose (sugar) in the body rise very high.
- The main feature of neonatal diabetes is being diagnosed with diabetes under the age of 6 months, and this is where it’s different from Type 1, as Type 1 doesn’t affect anyone under 6 months.
- As well as this, about 20 per cent of people with neonatal diabetes also have some developmental delay (eg muscle weakness, learning difficulties) and epilepsy.
- Neonatal diabetes is very rare, currently there are less than 100 people diagnosed with it in the UK.
- There are two types of neonatal diabetes – transient and permanent. As the name suggests, transient neonatal diabetes doesn’t last forever and usually resolves before the age of 12 months. But it usually recurs later on in life, generally during the teenage years. It accounts for 50-60 per cent of all cases. Permanent neonatal diabetes as you might expect, lasts forever and accounts for 40-50 per cent of all cases.
- Around 50 % of people with neonatal diabetes don’t need insulin and can be treated with a tablet called Glibenclamide instead. These people have a change in the KCNJ11 or ABCC8 gene and need higher doses of Glibenclamide than would be used to treat type 2 diabetes. As well as controlling blood glucose levels, Glibenclamide can also improve the symptoms of developmental delay. It’s important to know if you have/your child has neonatal diabetes to make sure you’re/they’re getting the right treatment and advice (eg stopping insulin).
- Genetic testing for neonatal diabetes is offered free of charge for all people diagnosed with diabetes before 9 months of age. Confirming the diagnosis by molecular genetic testing is essential before considering any change to treatment.
- More information about neonatal diabetes can be found here.
So if you were/your child was diagnosed with diabetes before you/they were 6 months old, ask your diabetes team for a test for neonatal diabetes. Your team can take a blood sample and send it to the Peninsula Medical School based at the Royal Devon and Exeter Hospital for analysis. The test is free. Go to www.diabetesgenes.org. This site will also tell your doctor how to take your blood and send it to the team at Exeter.