The end of May marked six months since I got CGM'd. WOW! It just flew by.
After two years of persistence, I finally got my CGM on November 27th 2015. When I announced this on social media I has a number of queries about how I managed to get approved and how difficult others were finding their quest.
As always, the one thing that the diabetes community is brilliant at, is sharing knowledge through our personal experiences for the benefit of others. So, here is the story of how I came to have a CGM.
How did this quest begin? Well, it began with an insulin pump (and that was another long drawn out "quest") in June 2010. I wrote about that journey here on 29th March 2011.
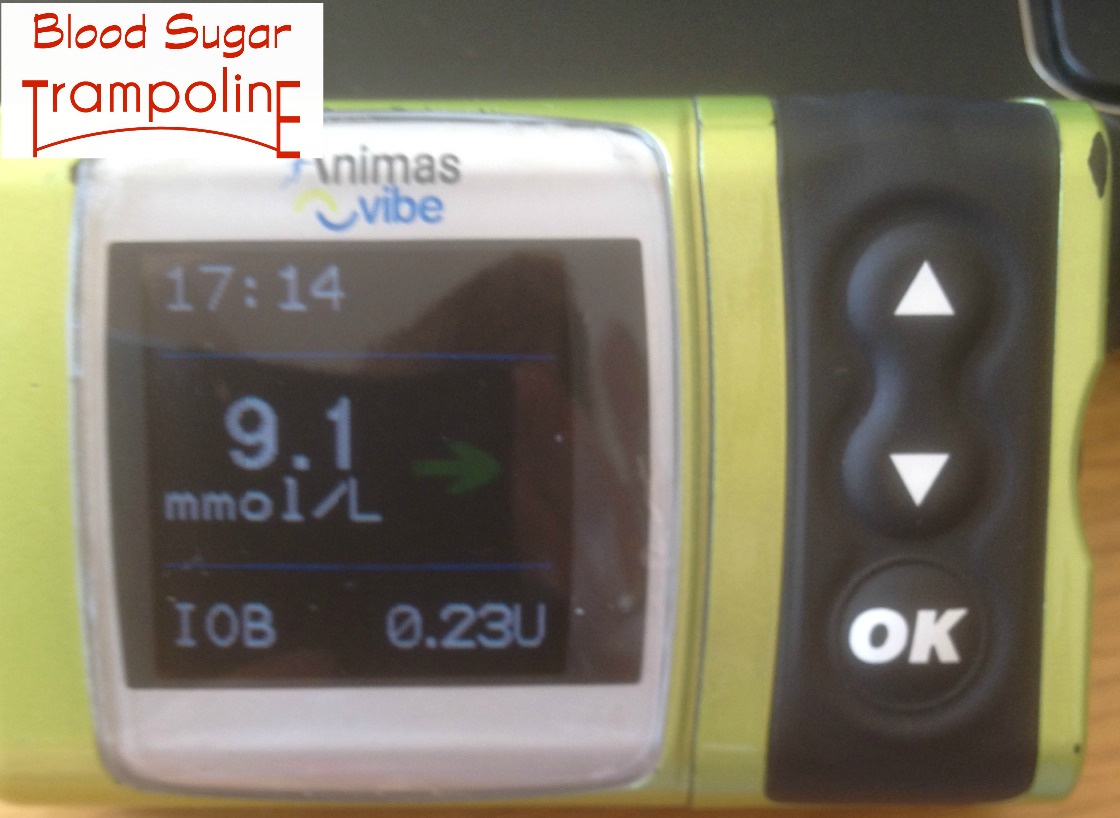
I use the Animas Insulin Pump and as soon as Animas announced that they were rolling out the Animas Vibe with CGM integration in the UK and Ireland, I was on it like sticky on a toddler.
My pump was due for an upgrade in 2014 as the warranty runs out at 4 years and because the pump software would not continue past January 2016. I called my Animas rep to find out how, or if there was a chance that I would get a Vibe as part of this upgrade and she said yes! Great! But wait!
Hiccup no. 1. However, between hearing this information and my next appointment at my endo's office, my Animas rep, the only Animas employee in Ireland at that time, took a 12 month sabbatical. That combined with having only 3 visits per year to my endo doesn’t give me much of a chance to get things done. I did get my Vibe in June 2014 and immediately started chasing down how to get the CGM component.
Hiccup no. 2. My Animas rep returned from her sabbatical the following August BUT then my fabulous endocrinologist left her position at the hospital I attend! I decided to use this opportunity to migrate back into public health care for my diabetes. My children were both in primary school and it was doable to fit clinic visits during school hours. I had also heard of a clinic that was only a one hour drive away that had an insulin pump clinic and DAFNE.
Hiccup no. 3. Fifteen month waiting list!!!!!!!!!!!!!!!! Not kidding! By the time I got my referral sorted out to my new clinic and waited I had been without medical care for 11 months. I was doing fine but I was starting to get a wee bit unsettled. Thankfully, when I called to chase up my referral they squeezed me into the Type 2 diabetes clinic in April 2015 but at least I was in and on the books.
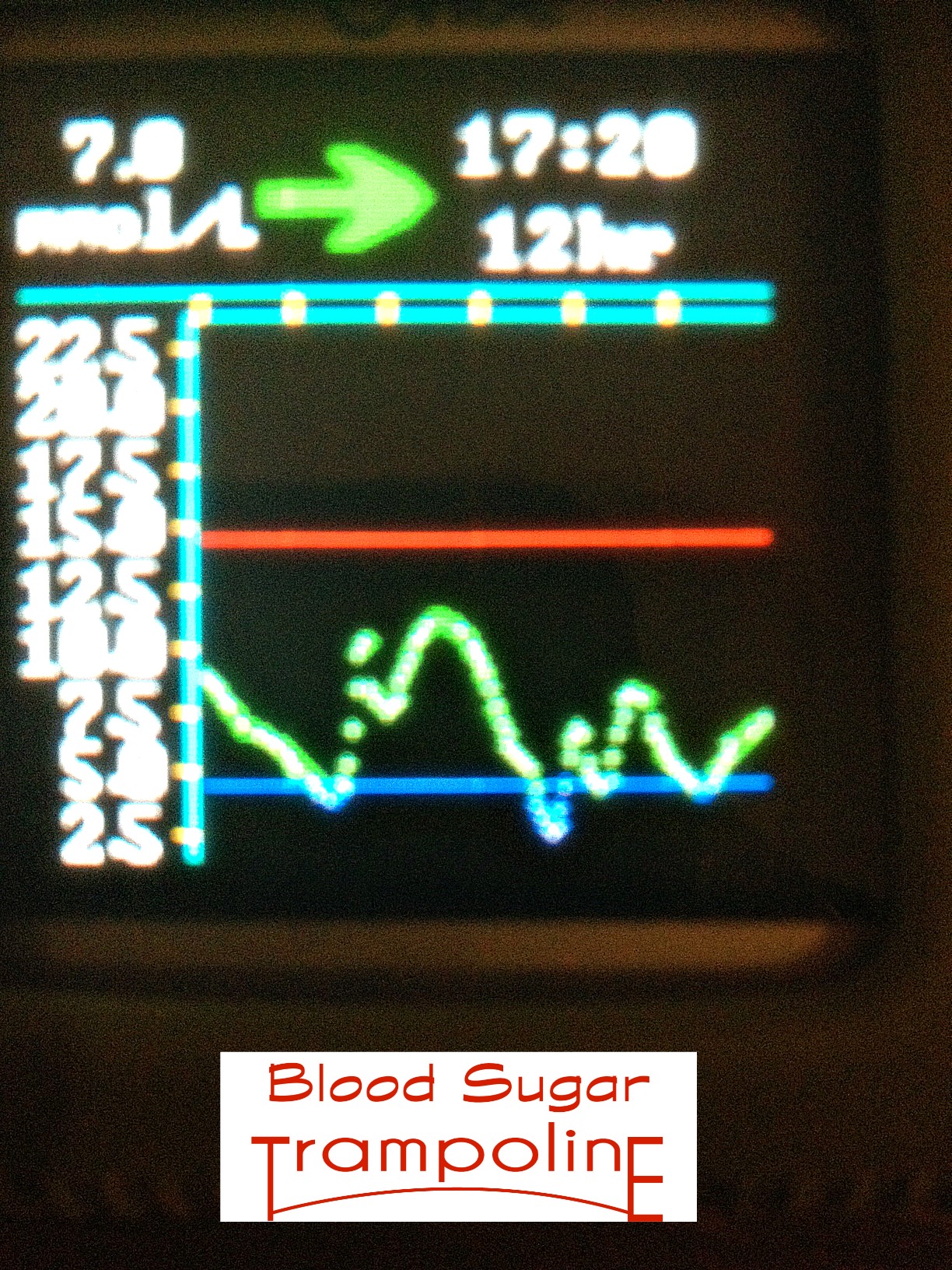
June 2015 - I set up a trial before purchase with a Dexcom CGM for two weeks and I was hooked. And now I had data, with the help of my mathematical husband, to strengthen my case for getting one permanently.
October 2015 - I presented my case and there were a couple of breakdowns in communication but the paperwork was put through to apply for funding approval from the HSE and on the 27th November I was live on a CGM permanently.
It took 17 months to complete this quest, that in the end when I had convinced my diabetes team why I wanted one took 6 weeks. Unlike an insulin pump, the training and education required before a patient goes live on a CGM is minimum.
In February 2016, an additional piece of this quest was completed and that was the reimbursement of the monthly supply of sensors which comes not from the Core List F of diabetes supplies and medications included in the Long Term Illness Scheme but on the Special Product List. See here for more information.
And that is the complicated story of how I got a CGM. My next post will focus on what I have learn about managing my diabetes by using it and how I will be taking it to the grave with me.
If you want to find out more about what is a CGM (Continuous Glucose Monitoring) device is, watch here. There are two available in Ireland at the moment; the aforementioned Dexcom (with or without the Vibe insulin pump) and the Medtronic RealTime Guardian CGM. The newer Medtronic pumps all come with CGM compatibility but you can get the CGM component without getting an insulin pump.






 However, I hear a lot of talk about ketones and began to think that, maybe, I'm a bit too relaxed about them and need to know a bit more.
However, I hear a lot of talk about ketones and began to think that, maybe, I'm a bit too relaxed about them and need to know a bit more.



