My diabetes diagnosis shattered my confidence in my ability to take care of myself, and my plan quickly became to just get through the rest of the term, move home for the summer to my previous summer job and figure the rest out over the summer. Adjusting to my new normal of living with diabetes began while I was still in hospital, or did it?
Docs and Nurses-The Whos Who of Diabetes Clinic
Sugar Tax and Diabetes
Making Sense of the Glycaemic Index
Mid October, I went to the DiabetesSisters Weekend for Women conference Alexandria, Virginia. See disclaimer at the end. One of the outstanding presentations I attended was by Thriveabetes 2016 speaker, Gary Scheiner’s presentation on “Making use of the Glycaemic Index”. This should not be a surprise to anyone has read Gary’s book “Think Like a Pancreas”. I will be honest here; when I heard the words “Glycaemic Index” I pretended I didn’t. And the reason is that several years ago, when it became a thing that was relevant to diabetes management, I tried to learn but I found it completely and utterly confusing. So I went to Gary’s talk as a skeptic.
BUT! As always Gary puts the information together well. See his blog posts here.
He started by saying that the glycemic index is the speed glucose enters the blood in the first two hours. It does not measure how fast foods enter the blood as glucose beyond that or how long it takes at all. A-ha! Ok so glycemic index is useful information for first two hours. I feel exonerated now.
This is hugely relevant to my diabetes management because I know that my rapid acting insulin peaks in approx 2 hours and that I might need additional insulin doses after that to cover the glucose released into my blood after the two hours.
The glycemic index is measured from 0 to 100. The closer to 100 a Food is, the higher its glycemic index is and the quicker the glucose hits your blood.
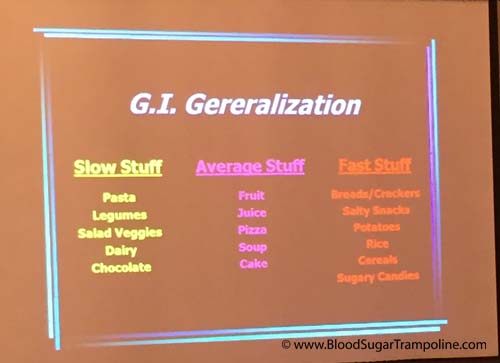
Here is a snapshot of the other things I learned;
- A mixed meal, ie a meal with protein, carbohydrates and or fat gravitates towards the carb. Meaning your body will process that first, albeit slower than if it was just carbs. So I might need to take a post meal dose of insulin in addition to my pre-meal dose.
- If you have a low GI food before your meal it will slow down the follow up starch in your meal. This is really good to know! Bring on the peanuts before the pasta or pizza :-)
- Larger portions take longer to digest. This isn’t new information to me but I suppose I always underestimate just how flippin’ long it takes.
- Time since your last meal affects the glycemic index. If you are still processing your food from the last meal, it’s going to slow down glucose absorption even more.

Some additional pieces of information not related to glycemic index but valuable.
- Don’t trust your CGM when you are recovering from a low. The lag time in full force.
- Insulin on board pump feature doesn’t take into account the food on board. As mentioned in the previous paragraph, if you are still digesting food you may need to override the insulin on board recommendation.
- Insulin resistance can happen if you have a meal with a lot of fat.
- Protein to insulin formula = ½ The total of protein grams and treat as carbs.
- Amylin/Symlin is a hormone that slows gastric emptying. People who don’t have insulin don’t have amylin either so stomachs process food quicker.
- Victoza is a GLP-1 injectable medication and reduces glucagon secretion; slows down the absorption of food.
In summary, glycemic index important to people with diabetes because:
- Satiety. Low glycemic index meals help you feel full for longer.
- Helps with the Timing of insulin. For example, if you know a meal or snack is going to have a high glycemic index then you could take your insulin 15 - 20. Minutes beforehand to give it a head start.
- Helps avoid post meal spikes
So, I’m glad that I learned all of this and I’m glad that I don’t have to waste any more of my time trying to figure it out because it makes more sense to me now. And It may help me to know the glycemic index of a Food I’ve never tried before so that I can figure how to deliver my insulin (pre-meal, at meal or extended Bolus).
Disclaimer: Diabetes Sisters paid for my conference registration and accommodation but also gave me a contribution towards my travel costs. All they asked for in return was that I would write a blog post about the conference which I had to do anyway because I learned so much that needs to be shared;-) And I wrote here about how I was selected.
Diabetes on steroids
Back in October, I had a steroid injection in my hip. And yes, it drove my glucose levels bananas! For those of you who may not be aware of it, steroids are one of the medications that truly mess up glucose numbers for lots and lots of people. The ultimate craziness only lasted two to three days but the residual crazy lingered a couple of weeks.
Here’s a little of the backstory behind why I got a steroid injection.
I have been complaining about my right hip for some time and I finally did something about it in September 2016. I went to my GP. He referred me to my physiotherapist and we did some “process of elimination” exercises. They didn't work. So then I went for an MRI and was referred to a rheumatologist.
At least now, we think I know what is wrong with my hip! It would seem both my physiotherapist and my rheumatologist agree that I have bursitis. And my rheumatologist injected steroids to reduce the swelling. If you have diabetes and you have steroids that plays absolute havoc with blood glucose.
However, no one could tell me how many days, weeks, months the glucose madness would go on for and how severe it would be.
Here is my experience of what happened to my glucose levels.
Prior to my injection my diabetes management was going fairly well with just the usual ups and downs. I had the shot mid morning and my glucose levels didn’t feel the effect of the injection until after lunch. But after lunch my numbers remained in the high teens until the early hours of the next morning. On day two, I noticed that if I increase my mealtime insulin significantly more than usual it would keep them in check. However, if I forgot to make the increase then I struggled to bring my numbers back down for hours.
Then the effect of the steroid started to wane slowly over the next two weeks and I had the opposite problem: trying to keep my glucose levels above hypo level. I adjusted insulin doses slowly and only making one or two changes at a time to bring them back to my normal diabetes levels (?!?!).
I was grateful that not only was I aware that this would more than likely happen but that both my endocrinologist, rheumatologist and physiotherapist reminded me it would. I'm probably going to have another dose in January but now, at least, I have a good idea of what to expect.
Weather the diabetes havoc-er
One of the factors not included in Diatribe’s 22 factors that influence glucose levels is the weather. Sometimes the weather plays with my diabetes management. And here’s how. Do you remember that really, really wet day we had last week? It seems like a distant memory now and I don’t think it had a name, like a storm name, but most of the country was flooded under a yellow weather warning.
When I got up that morning and look out the window I thought “Nope, I’m not walking, I don’t mind being wet and drippy but not that wet!” I was disappointed because most days I love my walk. It clears my head as I inhale clean fresh energy and exhale stress. I swing my arms vigorously and loosen up my neck and shoulders. I had missed my walk the day before due to a doctor's appointment so I was doubly disappointed.
So, with my daily constitutional off the menu, I took my “no-walk” breakfast insulin dose, which tends to be twice what I take if I am walking and off I drove the kids to school.
However, as I was dropping the teen and preteen to school the rain wasn’t that bad. So,I changed my mind (GASP)…. but how can I avoid a hypo seeing as I’ve taking all this insulin without using calories to prevent the low glucose reaction that will surely follow?
I decided to turn my background/basal insulin down to zero for one hour on my insulin pump. Yes, it was going to take an hour to take effect but it was better than a severe hypo. At least it might soften the blow.
Now, if I was on injection pens there is no way I could have avoided preventing a low without glucose.
So was I successful? Weeelll, kind of. I did have a hypo. A doosy at 2.8mmols but it didn’t feel as bad as it was and I didn’t feel like I had to consume the entire kitchen just about a dozen small jellies.
Compared to most hypos this one rebounded quite quickly and not too high. However, I did spend most of the day with glucose levels that were more elevated than my usual.
And there you have it, diabetes the spontaneity killer and weather the diabetes havoc-er.