My children have been back to school for almost two full weeks now and since their first day back I've been spending a couple of hours most days planning Thriveabetes 2018. A month ago, at our fundraiser, I was asked to explain what Thriveabetes is, why people with diabetes need it and why I was asking people to give money to it.
After my nerve wrecking speech, several people commented on how they had no idea that living with diabetes was so involved and required so much work. Why I keep forgetting this when I talk about my diabetes I'll never know!
This post is to explain to people who don't have diabetes, what living with type 1 diabetes is actually like, to explain what our conference does for people with diabetes, why I'm passionate about it and why I need it.
Here's what I said;
What is Thriveabetes? And why do people with diabetes need it?
To answer these questions I have to, first, take you on a little journey. My journey.
I was diagnosed with type 1 diabetes 24 years ago as a young adult and It changed my entire life. I'd like to be able to say that living with type 1 becomes easier but it doesn't - it becomes habit.
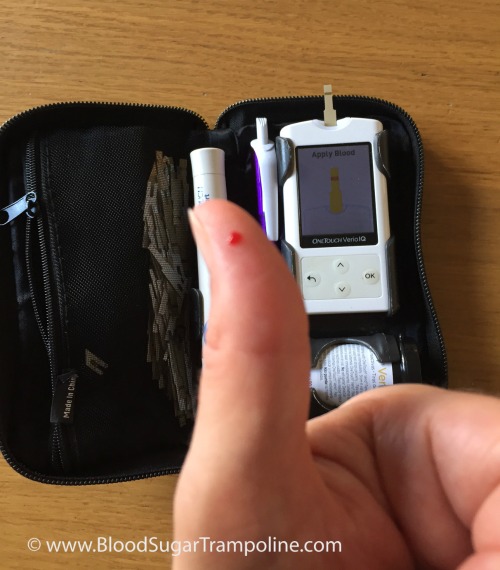
I woke up this morning, a little groggy because my glucose alarm went off during the night telling that my levels were a little high. So I got up, checked them on my meter, worked out a correction dose of insulin, took it and went back to sleep.
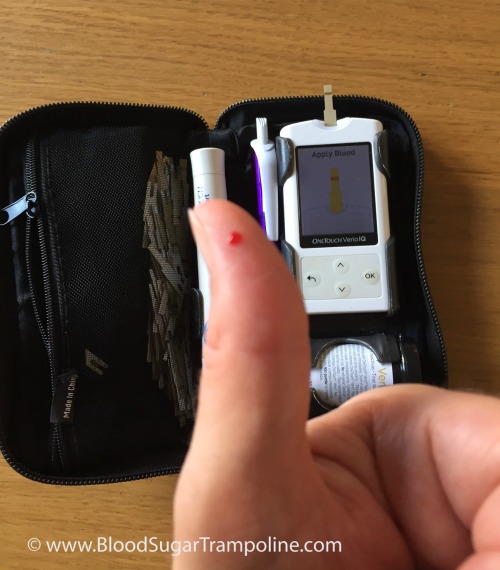 Before breakfast, I checked my levels again; they were in target, so I took my insulin for my regular weekend breakfast of tea and toast also known as 40g of carbs and then ate it.
Before breakfast, I checked my levels again; they were in target, so I took my insulin for my regular weekend breakfast of tea and toast also known as 40g of carbs and then ate it.
Two hours later with kids and car packed to travel across Ireland, I checked my levels again to see how close I came to getting it right. The answer was; not in target range, but close enough.
As I visited with my mother and family, I wondered what lunch was going to involve and when it was likely happen. It ended up being a sandwich at a Spar. I checked my glucose levels again. They were a little above my target, so I had to work out a correction dose of insulin plus working out an educated guess of how many grams of carbs were in this particular sandwich. Then I eat. My day, as with all other days, continued like this.
I do all of this out of habit. The numbers are very seldom perfect. But I get on with "close enough".
Now imagine, that the person with diabetes isn't you, but your child. So on top of all of those daily diabetes tasks that I do, you now have the added worry of “if I don't do this “close enough” my child is going to get sick. Again!”.
This kind of anxiety and stress goes on 24 hours a day, 7 days a week, etc. Diabetes NEVER takes time off. Ever.
This is why Thriveabetes is needed!
Thriveabetes is a place where you can relieve some of that stress and anxiety. The power and comfort of being in a room with so many people with diabetes, learning so much about managing daily life with it and knowing that every single person in that room knows diabetes like I do, lightens that load. There is no other place where we can get that.
It's a day that is organised completely by us; people with type 1 diabetes. We are all volunteers who are dedicated to and passionate about bring people with type 1 diabetes together to share what we deal with every day and to learn from world class speakers.
And that is Thriveabetes. And that is why I need it!




 When my children were younger, I was asked a couple of times about how I balance life as a mum and life as a person with type 1 diabetes. It was definitely a challenge to juggle parenting with anything but that's not news to any parent.
Now that my children are older (13 & 11) I can look back on what were the tough parts and what were the “advantages” of being a mum with type 1 diabetes.
When my children were younger, I was asked a couple of times about how I balance life as a mum and life as a person with type 1 diabetes. It was definitely a challenge to juggle parenting with anything but that's not news to any parent.
Now that my children are older (13 & 11) I can look back on what were the tough parts and what were the “advantages” of being a mum with type 1 diabetes.




