Last week was completely mental for me. Definitely not the life of a stay at home parent and way too exciting. Wednesday, a bunch of us diabetes advocates went to Leinster House to meet with our TD’s and Senators. This is the equivalent of meeting with congress in the US, kindof. I won’t go into detail here but if you're interested in what happened I posted about it here on Thriveabetes last Tuesday.
Thursday was the complete opposite, live moving from a developing country to a developed one. One day, I was asking government to approve the funding needed to improve our diabetes services, the next, I was in the world of research and science. Not a world I’m very comfortable in but I learned a lot about peer support and specifically this research project that Prof Sean Dinneen is leading on how to create a programme for young adults living with type 1 diabetes called D1 Now Study.
“This event was to provide a forum, lead by a diverse group of keynote speakers including Young Adult with T1D, for sharing experiences and developing ideas around the management of t1d during the challenging years of young adulthood.”
It was a jam-packed day with lots of international studies talked about from around the world about type 1 diabetes and their findings.
From The Role of Family in Supporting the Young Adult with Diabetes by Clea DeBrun Johansen from Denmark Diabetes Academy.
Among this study’s findings were that “The influence of the family continues to be very prominent during emerging adulthood, especially the college years.”
Her study also concluded that;
- Parents play an important, yet complex, role for emerging adults with type 1 diabetes.
- Parents can contribute positively to diabetes self-care and psychological well being.
- Parents can also negatively influence life with diabetes for emerging adults (absence, disinterest in diabetes, acting in a controlling manner).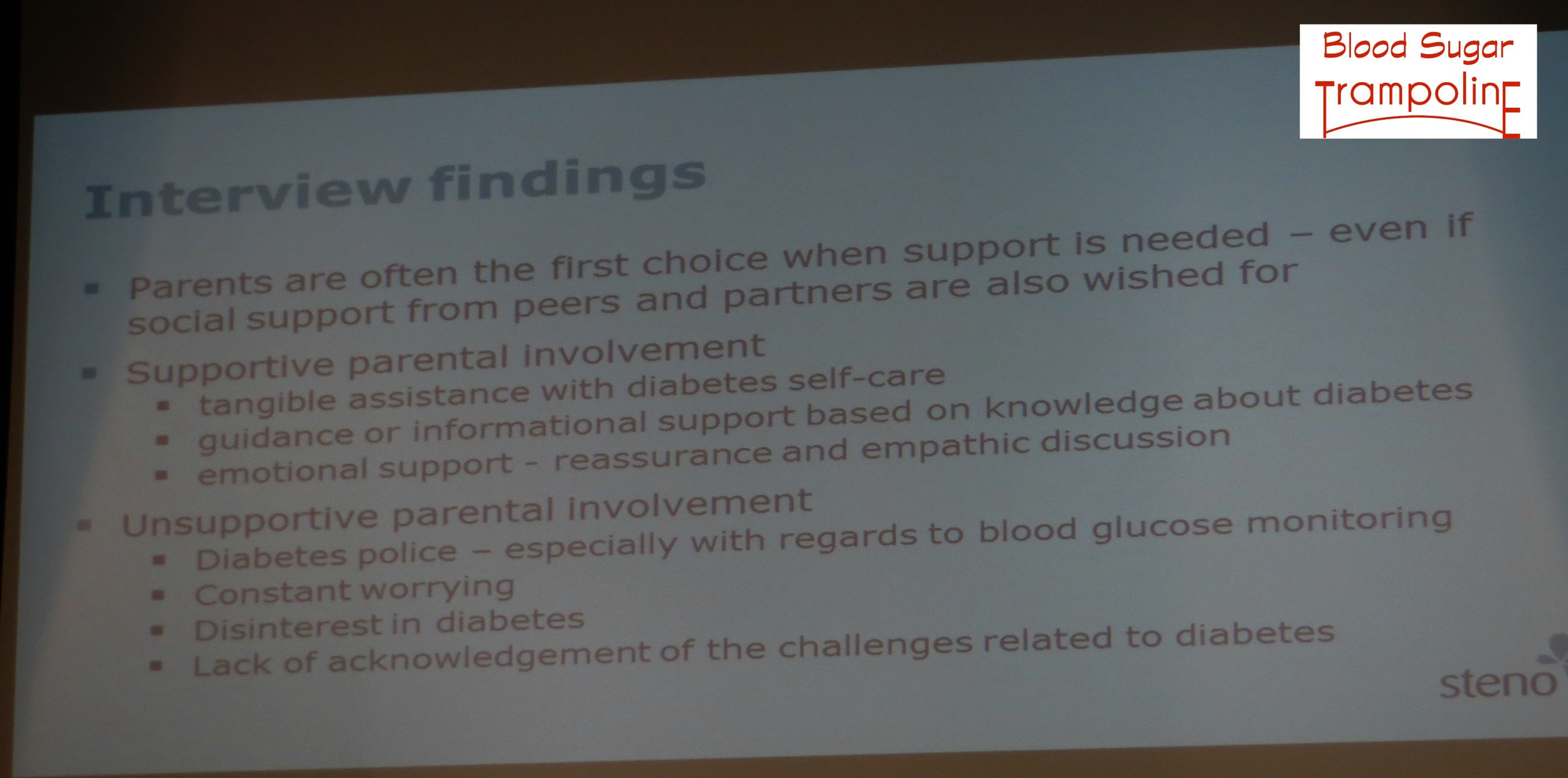 Emerging adults do not want to be too dependent on their parents - they want parents to be available when needed.
Emerging adults do not want to be too dependent on their parents - they want parents to be available when needed.
Clea ended with this quote but I would argue that you can do diabetes alone but nobody wants to.
Next up was Barbara Johnson who discussed WICKED, a new diabetes education programme in Sheffield. This has to be the coolest name for diabetes education. EVER!
Workin with Insulin, Carbs, Ketones and Exercise to manage Diabetes.
Prior to developing WICKED, Sheffield realised that young adults were taking responsibility for their diabetes often when changes are happening - starting work, moving away to uni, drinking alcohol, having sex and that they may not have received education targeted at them before. They asked for education that was relevant to them.
Will Hadfield from King's College Hospital, London, told us about their Transition Clinics for adolescents with diabetes.
His description sounded very much like an afterschool club with peer activities organised by the patients. He also mentioned that a large number of young adults don’t want to received anything diabetes related in their social media feeds. I can understand that they want to keep at least one zone or area of their lives free of diabetes. I have some of those too.
Sarah Simkin from Jigsaw Galway gave a very enlightening talk about how their
A Service Designed by Service Users.
From the design and layout of the building to how the service would be delivered. They really adopted the “Nothing about us, without us” motto that has been circulating for a couple of years and they owned it.
Young Adults with Diabetes Panel (YAP)
Then we heard from the first of two young adults with diabetes who are involved in the D1 Now study. Monica Mullins, a student in Galway, told of how she became a member of the Young Adult Panel (YAP) and the training they received to become researchers. There was a lot of training and it does make them more effective in the research but now I feel that they have altered their typical YA with diabetes demographic, making them not so typical now. Maybe an an additional YAP is needed so that they research team learn to communicate with them.
Our second voice of diabetes, Liam McMorrow designed a survey on “Understanding Young Adults preferences for Diabetes Clinic care”. It was really interesting and I had a couple of questions about his fantastic questionnaire but there wasn’t enough time to answer many questions.
CHOICE
Last but not least was David Chaney who is the National Director of Diabetes UK Northern Ireland and the only other Irish person I met at the Friend for Life Diabetes Conference in America last summer. David, with diabetes teams across Northern Ireland, developed CHOICE, (carbohydrate and insulin collaborative education). CHOICE is a structured education programme for children and young people with diabetes (aged 0-19 years) and their parents / carers.
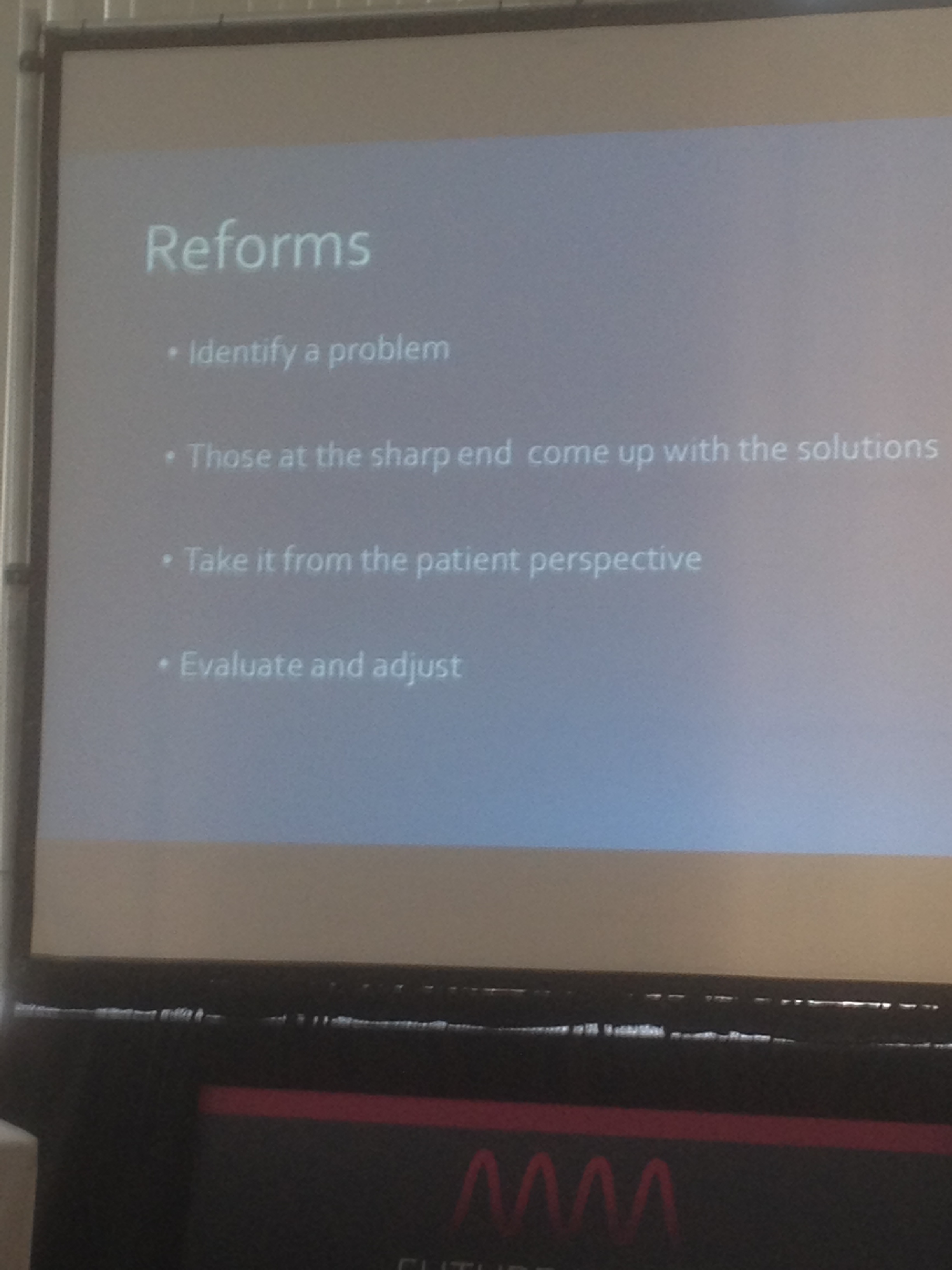
I don’t think there is a parent of a child with diabetes in Ireland who does not know about CHOICE. David took us on the journey of how CHOICE came to be and how it has developed and adapted to meet the needs of children and young people with diabetes.
He told us that when a child is diagnosed with diabetes all the education is directed towards the parents, so when a child transitions into the adolescent and young adult service we expect them to have absorbed all that information by osmosis. Barbara Johnson earlier reinforced this point. David believes, as many of us do, that diabetes education is the cornerstone to good diabetes management.
We are kind of putting our young adults with diabetes into the driving seat of their diabetes without giving them a few lessons and a bit of theory. But, you wouldn’t put a person in the driving seat without giving them a few lessons and a bit of theory first. Then as their confidence grows the diabetes team backs away but if there whenever they are needed. CHOICE is teaching adolescents and young adults to drive their own diabetes.
David also provide The Best Slide of the conference in my opinion. “If HCPs don’t provide diabetes education, others will” 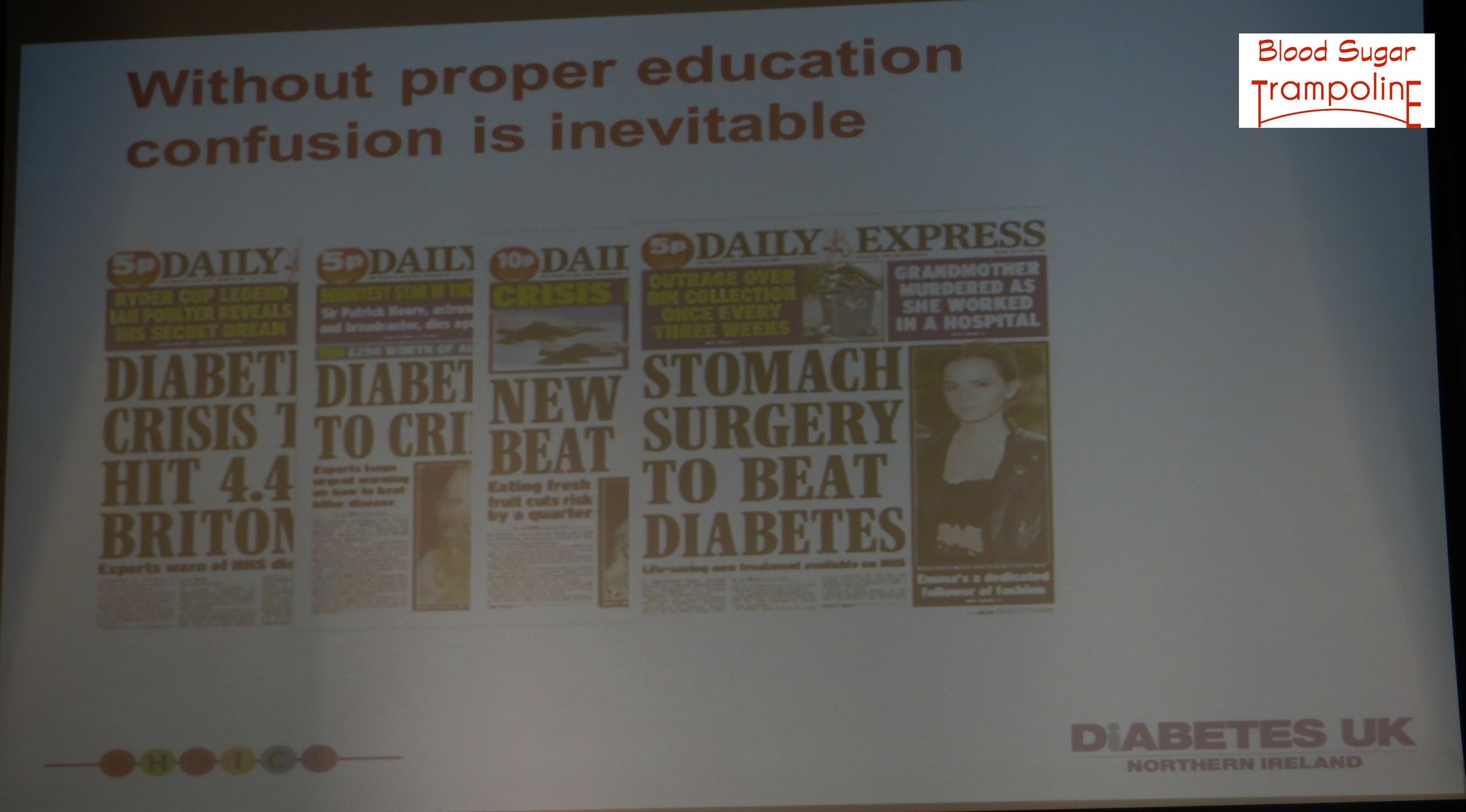
I did get a little frustrated and “irked” about half way through the conference because it was starting to feel like I was being talked about while in the room but not being included in the conversation. Maybe I needed some YAP training to fully participate? Again, it’s not a world I’m very familiar with so maybe that was it? I also wasn't able to attend the Hackathon that followed the Conference. And I am looking forward to seeing where the research goes and how it develops.
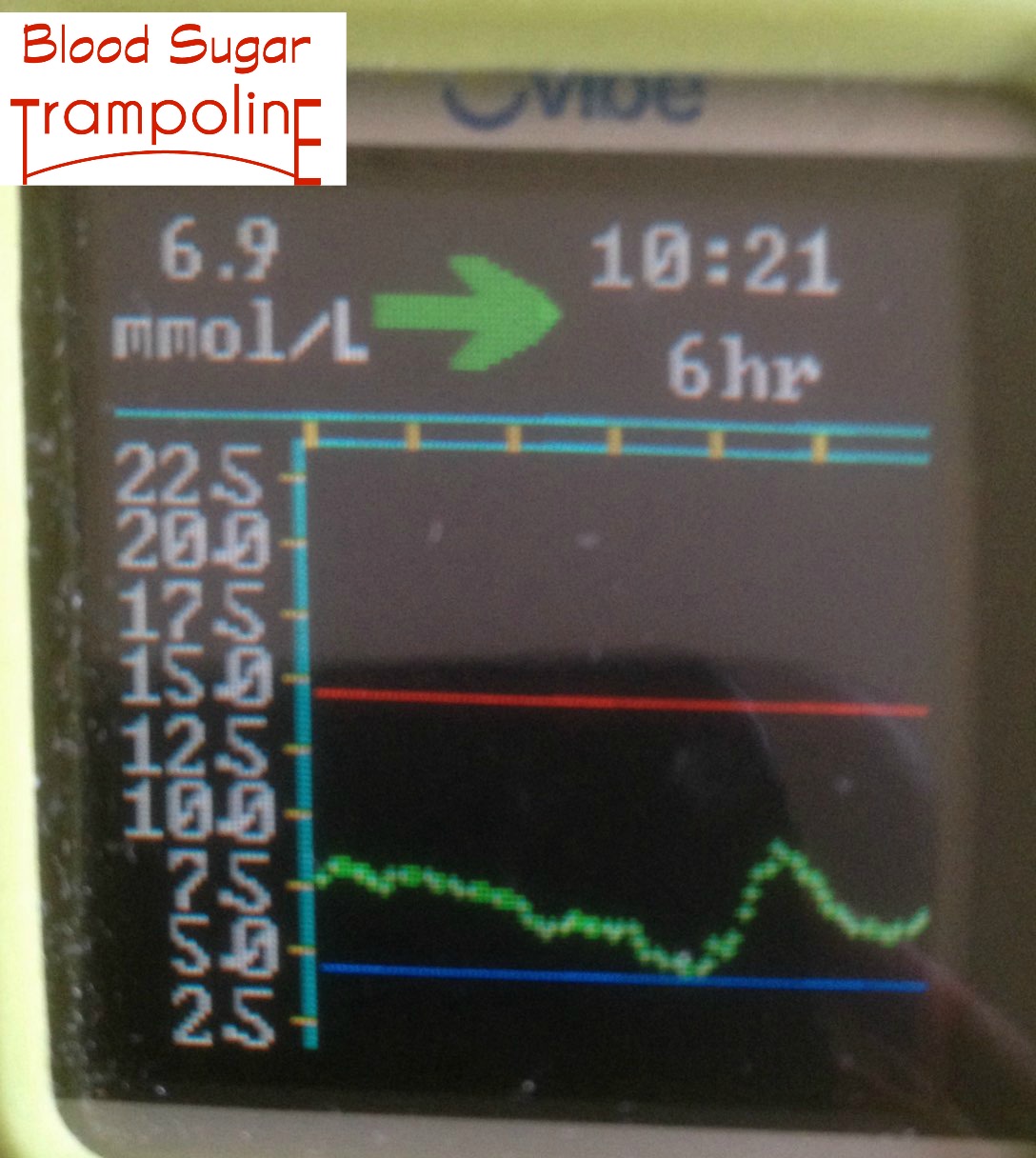
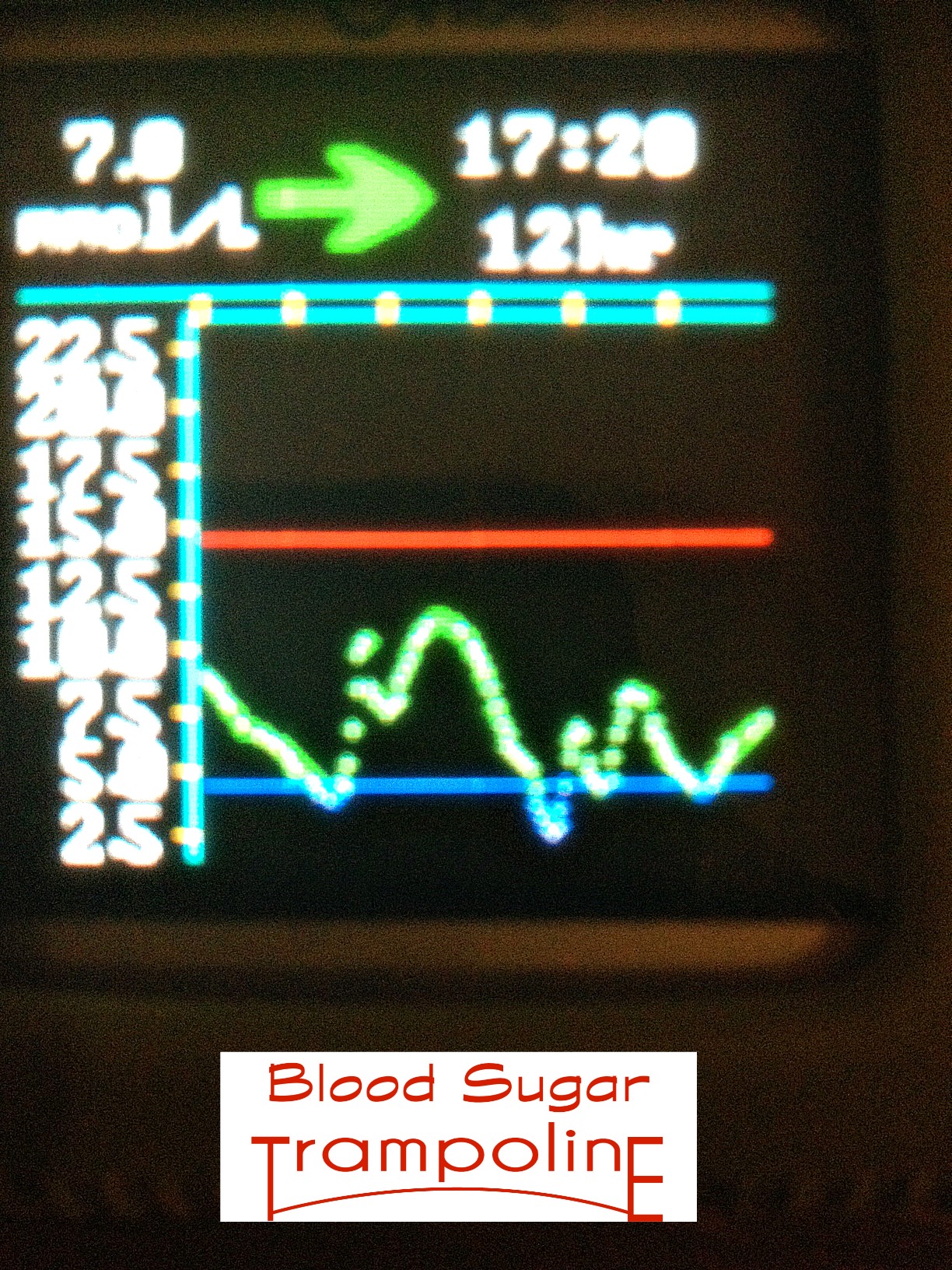
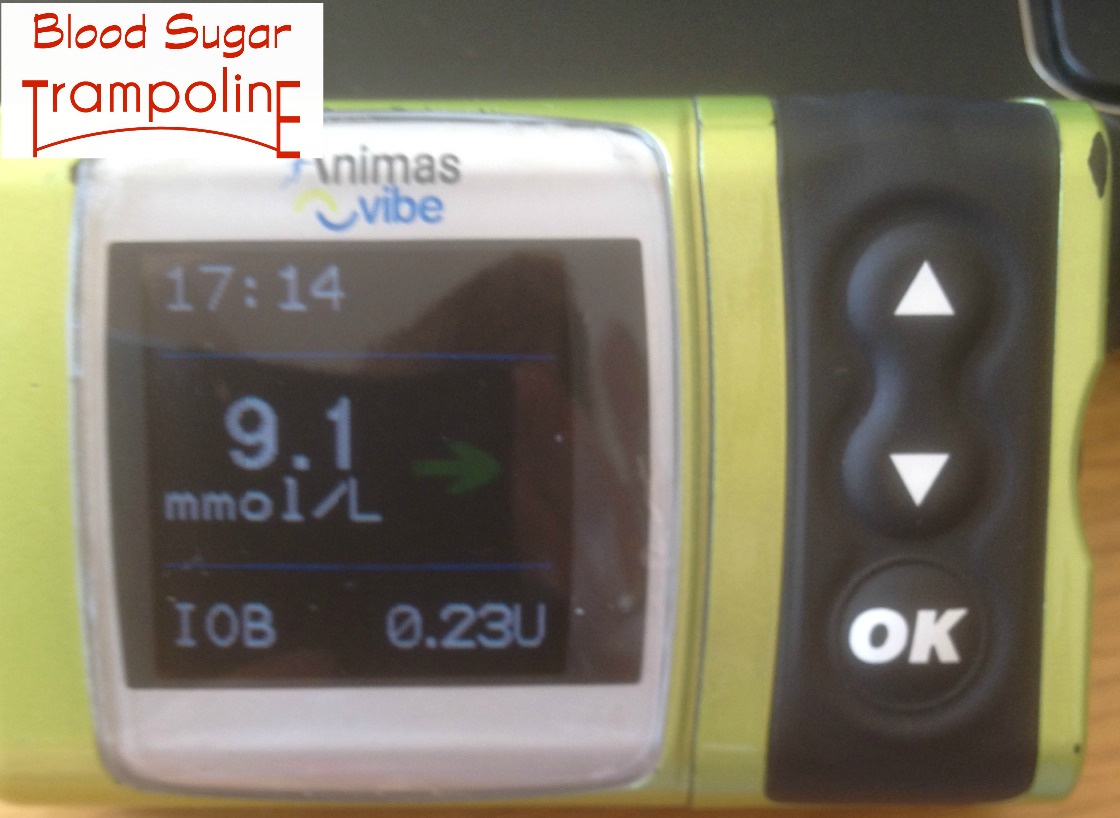
On a personal note the stress of travelling across the country, plus trying to find "volunteers" to look after my children had left the building, along with the high blood glucose numbers:-)