I have been using a Continuous Glucose Monitoring device (CGM) for six months and I feel that I have enough information now to share what I have learned about my diabetes management in those short months. A couple of weeks ago I shared how I came to get my hands on this little golden nugget and you can read about that here.
So here it goes, in no particular order, what I have learned.
Rapid acting insulin is not that rapid at all!
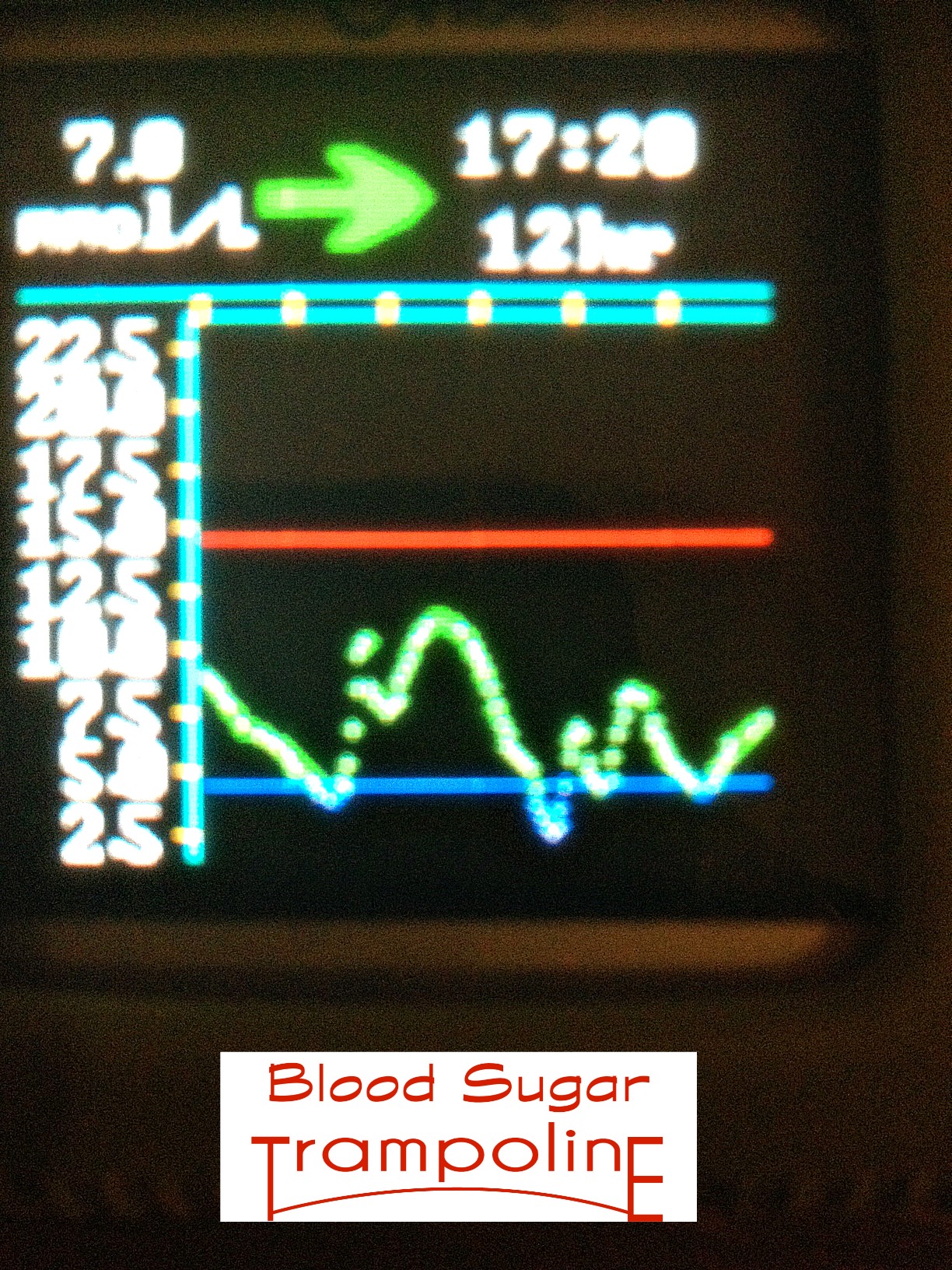
If my blood sugar levels dare to go ⇑ and beyond, it could take up to 4 - 6 hours for the insulin to bring them back to normal. It is a major exercise in patience!!! And can lead to rage bolusing (i.e. getting extremely frustrated and bolusing more that reason dictates).
Before CGM, I would take a correction dose of insulin, go to bed, only to wake up in the morning to realise that it hadn’t lowered my levels as much as I had hoped and I had spent at least 8 hours with elevated blood glucoses levels.
Hypo treatments don’t work fast either.
Glucose, even in its purest, most rapid form doesn't work fast enough. This can lead to over treating but thankfully the CGM can help curb the overtreatment.
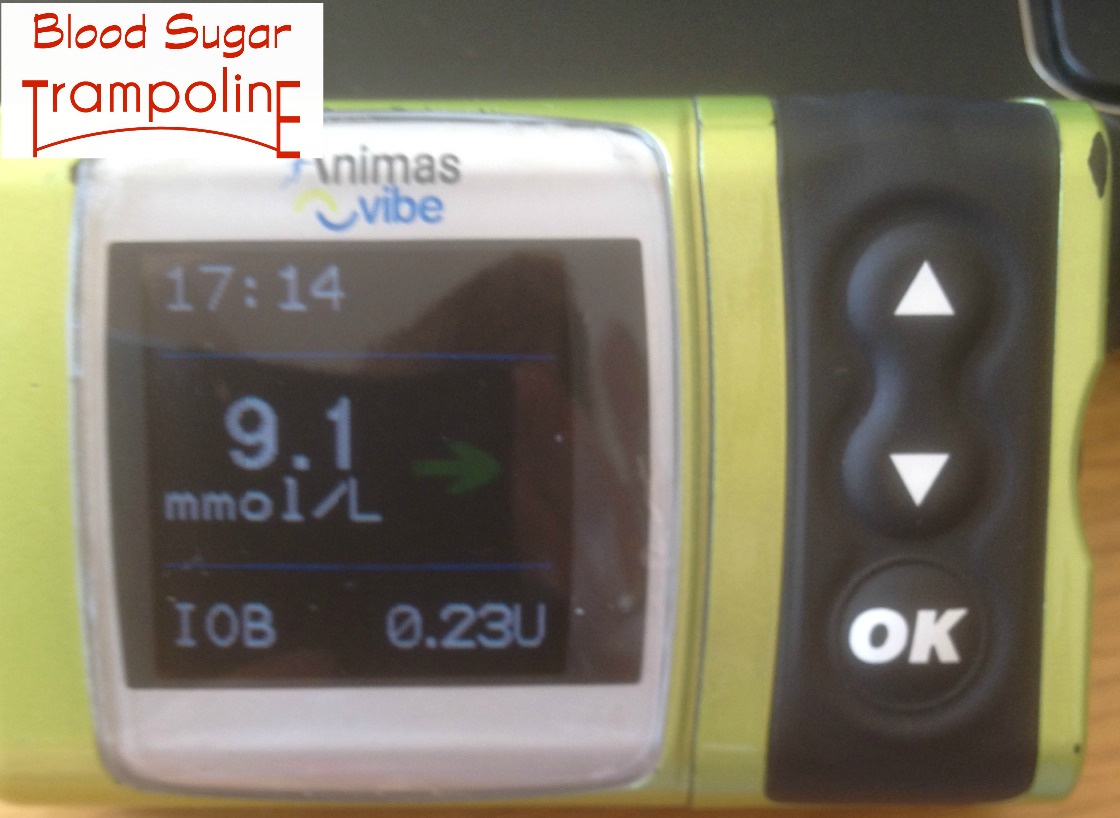
Angle of Arrow Interpretation ⇑⇒⇓⇖⇗⇘⇙
Interpreting what the angle of the arrow next to my blood glucose reading, means in terms of where my blood sugar levels are heading is not that easy but after a bit of trial and error can be achieved.
The alarms can be annoying.
The alarms! The alarms, in the beginning, were, can be annoying and did interrupt many nights of sleep. But they are there for a reason. And very good reasons at that.
The alarms are very useful learning tools.
I tried not to get frustrated with the alarms, especially the low glucose one, which I have set at 4.4mmols. This give me enough time to prevent an actual hypo and I’m still rational enough to decide how to deal with the impending train wreck.
Mostly I use the alarm as learning tool on how to adjust my insulin dose to avoid them. And it’s worked. Six months ago my high blood glucose alarm was set at 16.6 and now I’ve gradually brought that down to 13.3, it only very occasionally goes off (touch wood). They are especially helpful for dealing with days out of my routine and for food that I don’t have very often.
I’m self conscious about my gadgets and gizmos.
Since the weather warmed up I’ve been wearing short sleeves and my sensor, which is placed on my upper arm, attracts a bit of attention. This does make me think about wardrobe choices a bit more and if I really want to talk diabetes.
I sleep less.
This is both good and bad. Bad because I might be woken several times a night because of the alarms and good because I know that I will never have a hypo again without being aware of it. Sleeping through hypos was a huge concern of mine and the reassurance that my CGM gives me is invaluable.
Sometimes my CGM is not reliable.
Just like any other piece of technology I have noticed that there are times where I should double check my CGM reading with a finger prick check. The times this most often happens is usually the first day of a new sensor and when my blood glucose levels are rising quickly or falling quickly. So I still do 7 finger prick tests a day.
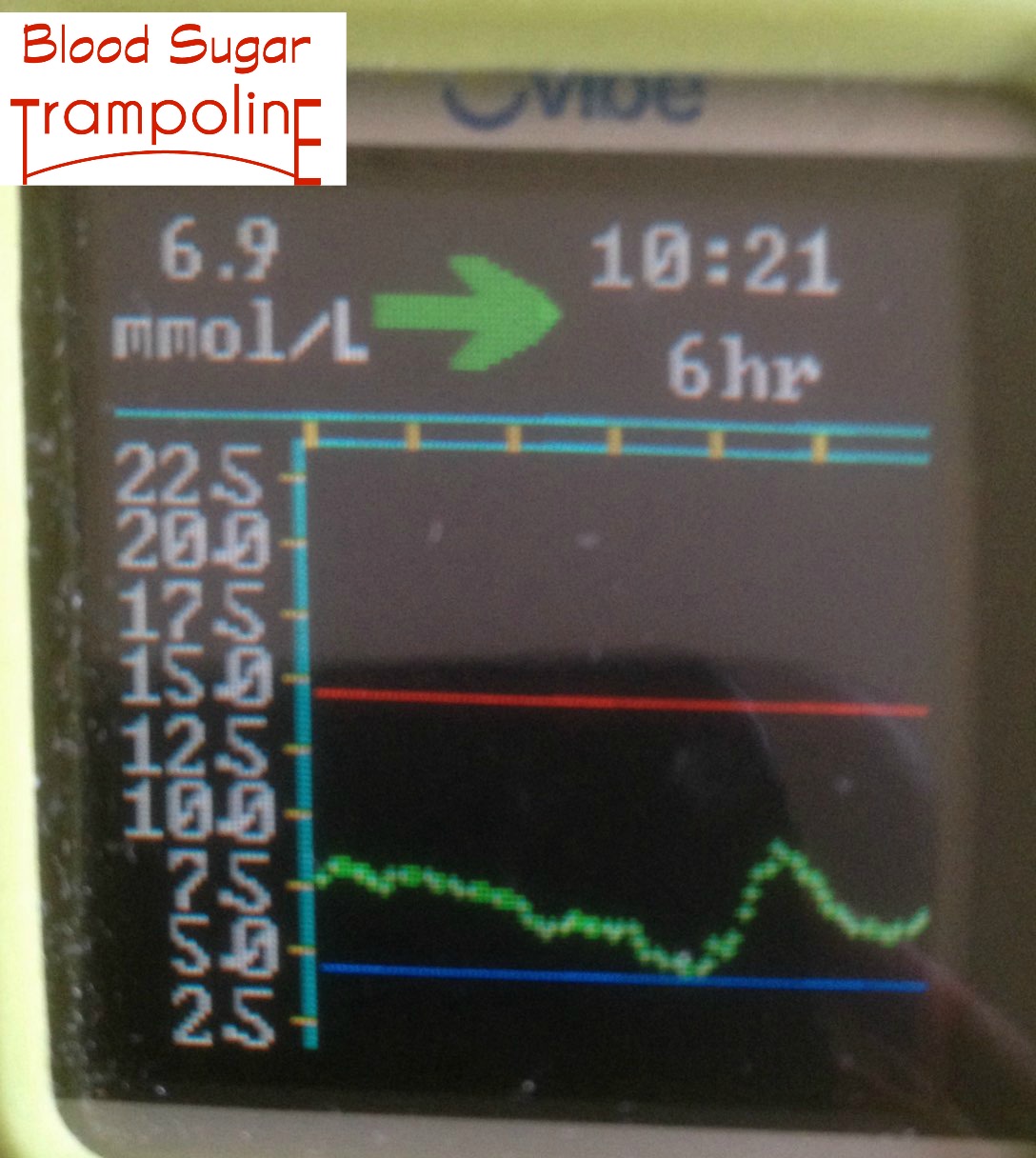
My blood glucose levels are within their targets 65% of the time.
Finger prick blood glucose tests give you a snapshot of where your levels are at that point. The CGM tells you where your blood glucose levels are ALL of the time. It’s the difference between having a photo or seeing the whole movie/book. Now that I have a starting point I can try to increase that percentage and spend more time within a healthier blood glucose range. I also appreciate knowing that number is over 50%.
My CGM does influence my behaviour.
That little graph display does influence my behaviour around food and it also helps me stem the spike in my post meal blood glucose levels. It influences decisions about my treats, such as helping me determine should I choose a full bar of chocolate, just 2 squares of the good dark stuff or on warm sunny days the ice cream. My cgm really helps me spend more time within my blood glucose target range.
It has helped reduce my HbA1c!!!
Yes! I had my lab work done at the end of May and I have had the lowest HbA1c that I have had in four years and the time before that I maintained close to this level while I was pregnant with my first child 12 years ago. I have not been able to stabilize this level at any other time. I have been using an insulin pump for 6 years and hadn’t achieved a lower number. Insulin pumps should be available to those who want them and it should be very much about a personal choice. But CGM’s, in my opinion, are way more valuable a tool for managing diabetes and should be strongly encouraged. Even if it’s just for a couple of months. I know they are expensive but in the long run they would reduce the number of hospital admissions for both hyper and hypoglycemia.
All in all, I am never giving this device up! Knowing where my blood sugars are at any given time has been so reassuring and relieved so much anxiety.
On a promotional note, I attended a presentation by Thriveabetes 2016 keynote speaker, Gary Scheiner on "Making the Most of Your CGM" where I learned lots of useful information and he has published a book on it, "Practical CGM". You can register for Thriveabetes 2016 here.