There are lots of people on social media doing their bit for diabetes awareness, and this is fantastic. However, raising awareness seems to be a big buzzword these days, but what does that really mean, and how do we raise awareness of something effectively? Should I do it by sharing a random image on my Facebook feed that doesn’t tell any of my friends anything at all? Or should I use my social media to share information?
November is Diabetes Awareness Month
Docs and Nurses-The Whos Who of Diabetes Clinic
HSE Discriminates Against People with Type 1 Diabetes
The HSE discriminates against people with type 1 diabetes on the Freestyle Libre reimbursement scheme announced on January 19th 2018. The HSE states that it bases it recommendations on the Health Technology Assessment Group (HTAG) Advice Note so “that numbers being treated do not exceed that expected”.
The HTAG Advice Note recommends that:
“Careful patient selection should be part of the agreement, with hospital consultant initiation, and preference for children and young adults in the first instance so that numbers being treated do not exceed that expected, despite the lack of clinical evidence that the Freestyle Libre is beneficial for this group.
I completely support taking a phased approach to this scheme as nobody knows how much it’s going to cost or save and this is a brand new scheme that will need to be tweaked.
Service Providers Must Make Reasonable Accommodations
However, there were many, many, many ways the HSE could have found to phase in the Freestyle Libre, in addition to clinical need but not limited by age. I can think of three straight away that would also not not allow the numbers of users to exceed expectations.
In fact, “The law which deals with disability in the provision of goods and services is the Equal Status Acts 2000-2015 (ESA) “says that service providers must make reasonable accommodations so that people with disabilities can use services like everyone else (Source - Human Rights Equality Commision).
I would actually argue that a person growing a tiny human in their dysfunctional body or a person who is on the verge of developing diabetic complications should be included.
Maybe a person with a medical card who would otherwise never afford this device should be prioritised?
Or person who is required to do SMBG testing "more than 10 times a day if this is necessary because of the person's lifestyle (for example, driving for a long period of time, undertaking high-risk activity or occupation, travel)." Source: UK NICE Guidelines. The NHS have issued similar guidelines to the Regional Medicines Optimisation Committee (RMOC) on who should be reimbursed for Flash Glucose Monitoring Systems.
Lacks Clinical Evidence to Support Recommendations
The HTAG document makes it’s recommendation that this device be approved for children without any clinical evidence to support it.
It completely contradicts itself by saying that none of the clinical trials used to based their recommendations on had children as participants, that they are “unclear whether data from these (clinical trials Bolinder et al. 2016; Haak et al. 2017) trials are generalizable to children.” The HTAG acknowledges that “There is limited data to support the routine use in people who are less well managed or in children and young people.”
Yet this is the group they recommend. The HSE have chosen to ignore the clinical evidence from two clinical trials of the many, many benefits to adults on MDI.
“Careful patient selection should be part of the agreement, with hospital consultant initiation, and preference for children and young adults in the first instance so that numbers being treated do not exceed that expected.”
They also chose to ignore the Expert Opinions who:
“consider the product would be of benefit to all patients with diabetes using multiple daily injections, however those who would benefit the most include:
- Young people with type 1 diabetes
- Parents or carers of children with type 1 diabetes
- People who struggle with SMBG
- People who lead active lives
- People who have poor hypoglycaemic awareness”.
Continuing Discriminatory Pattern towards Adults with Type 1 Diabetes
This is not the first time that the HSE have discriminated against adults with type 1 diabetes. Adults have been excluded from standard access to insulin pumps and from standard diabetes education so “that numbers being treated do not exceed that expected”. And now, the Freestyle Libre.
When will the 13,000 Adults with Type 1 diabetes have the same provision of medical devices and services as children with type 1 diabetes?
When will our HSE and our government stop viewing us as a financial drain on the healthcare budget and finally see adults with type 1 diabetes as people worth investing in?
The HTAG document was published on the 11th November 2017 and can be found here. As of 3pm Thursday 15th February, this document has been taken off he HSE website, if you would like to view it you can do so here.
I posted my initial reaction to the HSE’s announcement here if you need background information.
See this post from Thriveabetes on what is happening with the Equality for all People with type 1 diabetes campaign.
Freestyle Libre Access For All
Making Sense of the Glycaemic Index
Mid October, I went to the DiabetesSisters Weekend for Women conference Alexandria, Virginia. See disclaimer at the end. One of the outstanding presentations I attended was by Thriveabetes 2016 speaker, Gary Scheiner’s presentation on “Making use of the Glycaemic Index”. This should not be a surprise to anyone has read Gary’s book “Think Like a Pancreas”. I will be honest here; when I heard the words “Glycaemic Index” I pretended I didn’t. And the reason is that several years ago, when it became a thing that was relevant to diabetes management, I tried to learn but I found it completely and utterly confusing. So I went to Gary’s talk as a skeptic.
BUT! As always Gary puts the information together well. See his blog posts here.
He started by saying that the glycemic index is the speed glucose enters the blood in the first two hours. It does not measure how fast foods enter the blood as glucose beyond that or how long it takes at all. A-ha! Ok so glycemic index is useful information for first two hours. I feel exonerated now.
This is hugely relevant to my diabetes management because I know that my rapid acting insulin peaks in approx 2 hours and that I might need additional insulin doses after that to cover the glucose released into my blood after the two hours.
The glycemic index is measured from 0 to 100. The closer to 100 a Food is, the higher its glycemic index is and the quicker the glucose hits your blood.
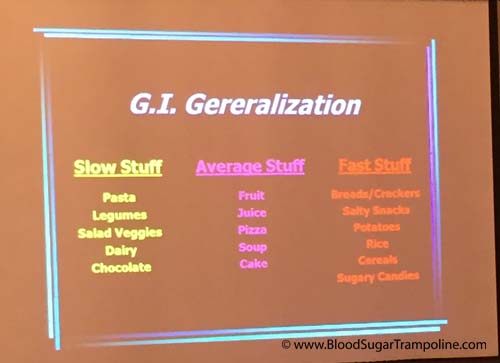
Here is a snapshot of the other things I learned;
- A mixed meal, ie a meal with protein, carbohydrates and or fat gravitates towards the carb. Meaning your body will process that first, albeit slower than if it was just carbs. So I might need to take a post meal dose of insulin in addition to my pre-meal dose.
- If you have a low GI food before your meal it will slow down the follow up starch in your meal. This is really good to know! Bring on the peanuts before the pasta or pizza :-)
- Larger portions take longer to digest. This isn’t new information to me but I suppose I always underestimate just how flippin’ long it takes.
- Time since your last meal affects the glycemic index. If you are still processing your food from the last meal, it’s going to slow down glucose absorption even more.

Some additional pieces of information not related to glycemic index but valuable.
- Don’t trust your CGM when you are recovering from a low. The lag time in full force.
- Insulin on board pump feature doesn’t take into account the food on board. As mentioned in the previous paragraph, if you are still digesting food you may need to override the insulin on board recommendation.
- Insulin resistance can happen if you have a meal with a lot of fat.
- Protein to insulin formula = ½ The total of protein grams and treat as carbs.
- Amylin/Symlin is a hormone that slows gastric emptying. People who don’t have insulin don’t have amylin either so stomachs process food quicker.
- Victoza is a GLP-1 injectable medication and reduces glucagon secretion; slows down the absorption of food.
In summary, glycemic index important to people with diabetes because:
- Satiety. Low glycemic index meals help you feel full for longer.
- Helps with the Timing of insulin. For example, if you know a meal or snack is going to have a high glycemic index then you could take your insulin 15 - 20. Minutes beforehand to give it a head start.
- Helps avoid post meal spikes
So, I’m glad that I learned all of this and I’m glad that I don’t have to waste any more of my time trying to figure it out because it makes more sense to me now. And It may help me to know the glycemic index of a Food I’ve never tried before so that I can figure how to deliver my insulin (pre-meal, at meal or extended Bolus).
Disclaimer: Diabetes Sisters paid for my conference registration and accommodation but also gave me a contribution towards my travel costs. All they asked for in return was that I would write a blog post about the conference which I had to do anyway because I learned so much that needs to be shared;-) And I wrote here about how I was selected.