Last week, our local type 1 diabetes support group organised a talk on heart disease and it’s association with type 1 diabetes (with a great speaker and a good crowd - thanks to all who attended). I feel that out of all the complications of diabetes it’s not talked about as much as the diabetic retinopathy, foot disease or kidney disease complications.
Yet, I also feel that it’s the sneakiest of all the complications. There are warning signs for diabetic retinopathy, foot disease or kidney disease and, in today’s world, it is possible to maybe halt the progression of these complications.
But unless you are paying close attention to all the risk factors; high blood pressure, high cholesterol, family history and the lifestyle factors, it can seem like it comes from nowhere. Not to mention that better glycemic management is linked to weight gain, which increases our risk again! Yeah, right - how can we win?
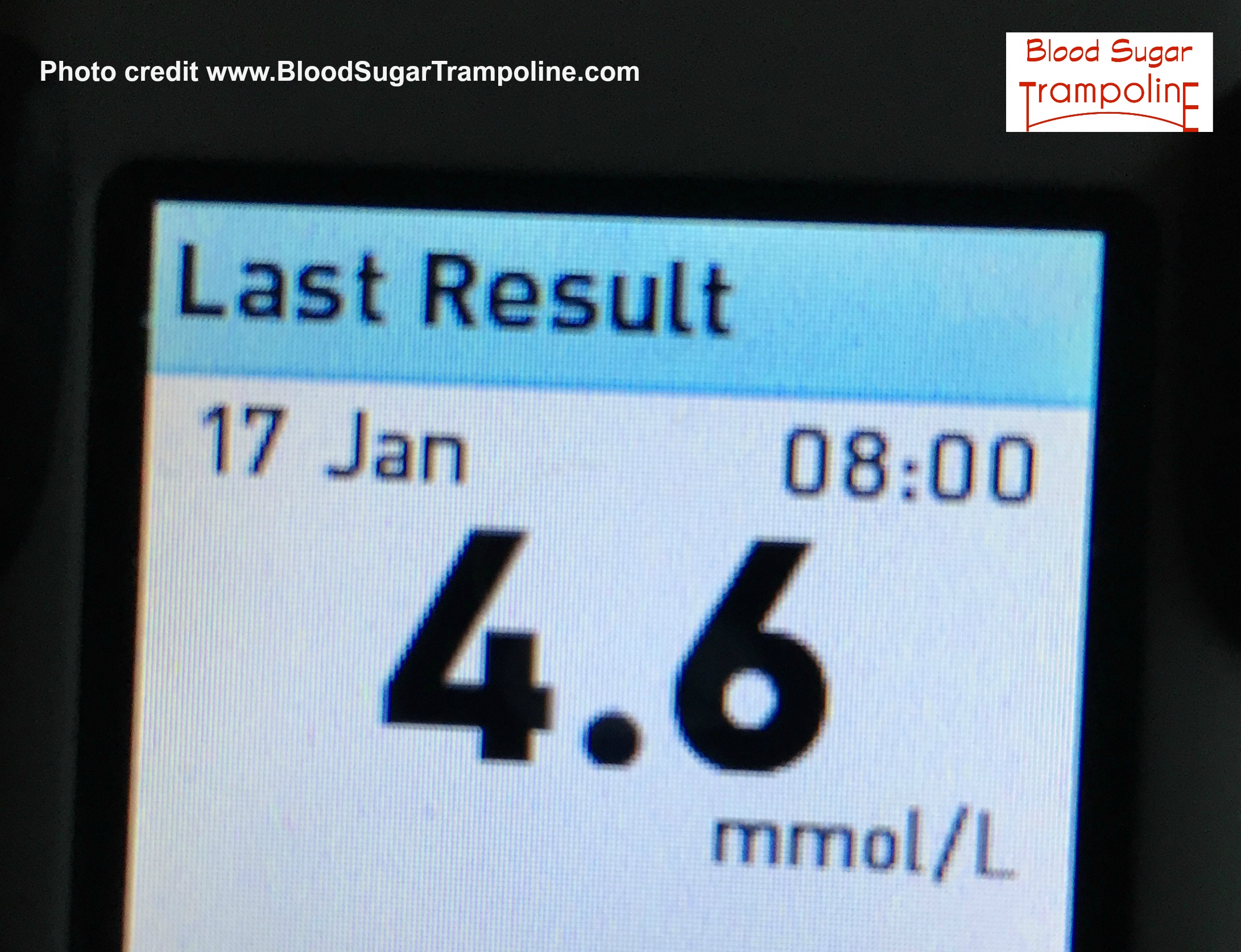
I also was under the impression that because I eat healthily and exercise I had that box firmly ticked and didn’t have to worry about heart disease. That heart disease related more to people with type 2 diabetes. A cholesterol level of 5.7 told me otherwise.
And then I found this; “Heart attacks and other cardiovascular complications cause the death of nearly 3 out of every 4 people with type 1 diabetes, compared with just 1 in 4 people in the general population.” according to a Swedish study published online September 18 2015 in medical publication; Lancet Diabetes & Endocrinology.
Dang it - I should always question what I think I know!
Our speaker was very concerned about giving us negative and scary information. But I was like "bring it"! I was not scared or running from the room hysterically. And I was surprised at my reaction.
All this information might seem like it’s scaremongering. But I was not scared or running from the room hysterically. P.S. I do firmly believe that fear is not a good motivator for anybody!!!
When I was younger, I really didn’t want to hear about the worst case scenarios. Those nasty complications that would happen to me if I didn’t do as I was told. I didn’t want to know about what could happen down the road.
Well, I seem to be at that point “down the road” where information, even scary information, gives me power over it. At our presentation, I was calmly thinking to myself “it’s good that I know this” and “it’s not going to catch me out because I know this scary diabetes heart stuff now”.
It feels strange now that information about what were once “scary diabetes complications” is now information that gives me power over my diabetes. This information empowers me to stay healthy… but I was also ready to hear it.





 New year's resolutions are a distant memory as is a reason, as good as any, for some people to have a new beginning. And, apparently, that only ever means a diet, maybe a gym membership that never gets used and a bombardment of media ads to be healthy, get fit and go on a diet. I felt this year it was more annoying than usual. I actually have a friend who refuses to buy a women's magazine for the months of December and January for this reason!
New year's resolutions are a distant memory as is a reason, as good as any, for some people to have a new beginning. And, apparently, that only ever means a diet, maybe a gym membership that never gets used and a bombardment of media ads to be healthy, get fit and go on a diet. I felt this year it was more annoying than usual. I actually have a friend who refuses to buy a women's magazine for the months of December and January for this reason!
 I feel like I should’ve gone all out and had the muffin. But at least this job is done for another year.
I feel like I should’ve gone all out and had the muffin. But at least this job is done for another year.