I have lived with Type 1 Diabetes for 23 years. I know how lucky I am to not have any diabetes complications…. so far. And yes, a decent HbA1c does play a role in that, but more than we want to think about it, some of it is down to luck. However, it is a lot of hard work to pull off a decent HbA1c and people are very often surprised when I tell them all the things I do to try to achieve that. Maybe I make it look easy? Or maybe they’re wishing for something easy, but the easy life died along with our pancrea.
However, it is a lot of hard work to pull off a decent HbA1c and people are very often surprised when I tell them all the things I do to try to achieve that. Maybe I make it look easy? Or maybe they’re wishing for something easy, but the easy life died along with our pancrea.
So, how do I manage my diabetes?
Managing diabetes is not as simple as taking my insulin and forgetting about it. I don’t just think about my type 1 diabetes at mealtimes - I can’t afford to, so much can happen in between meals.
In my opinion, managing diabetes is about balancing medication and physical activity with carbohydrate intake and stress levels. Even if I lived every single day the same this would be difficult because of the variables like stress, illness hormones, climate changes, etc.
Here is the “Magic” list of things I do to “manage” my diabetes.
- Blood Glucose monitoring:
- at least 7 times a day. Before I take insulin which would be every time I eat. And I check about 2 hours after to be reassured that I didn’t take too much or too little insulin.
- at least 7 times a day. Before I take insulin which would be every time I eat. And I check about 2 hours after to be reassured that I didn’t take too much or too little insulin.
- Taking insulin:
- I take at least 3 bolus infusions daily through my insulin pump. I may do an extra fraction of a unit in between those times if needed. My basal/background insulin is delivered continuously through my insulin pump.
- Carbohydrate counting:
- I’m hopeless at eyeballing the amount of carbohydrate on my plate so I weigh it. I find that my measuring the amount of carbohydrate, my insulin to carb ratio is more accurate.
- Record keeping:
- there’s a lot to keep record of. I’m a recent convert to a smartphone so I haven’t completely let go of pen and paper to keep track of everything, but I do use an app that makes me feel good about logging information and sends me a weekly email with how I’m doing.
- Physical activity:
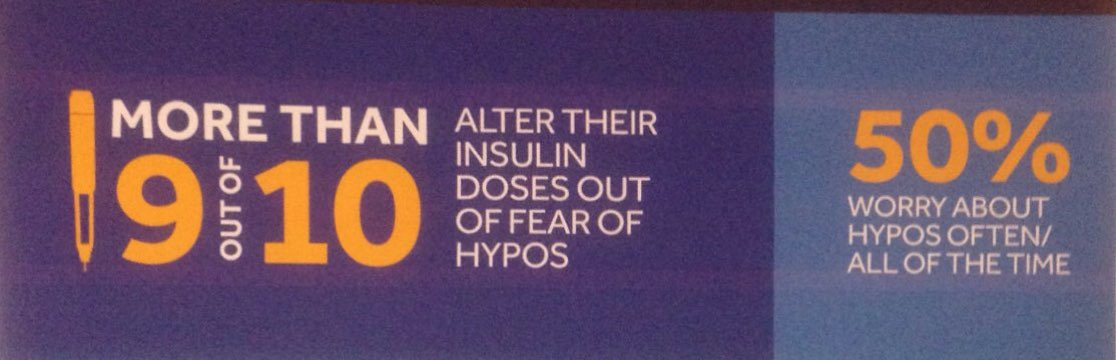
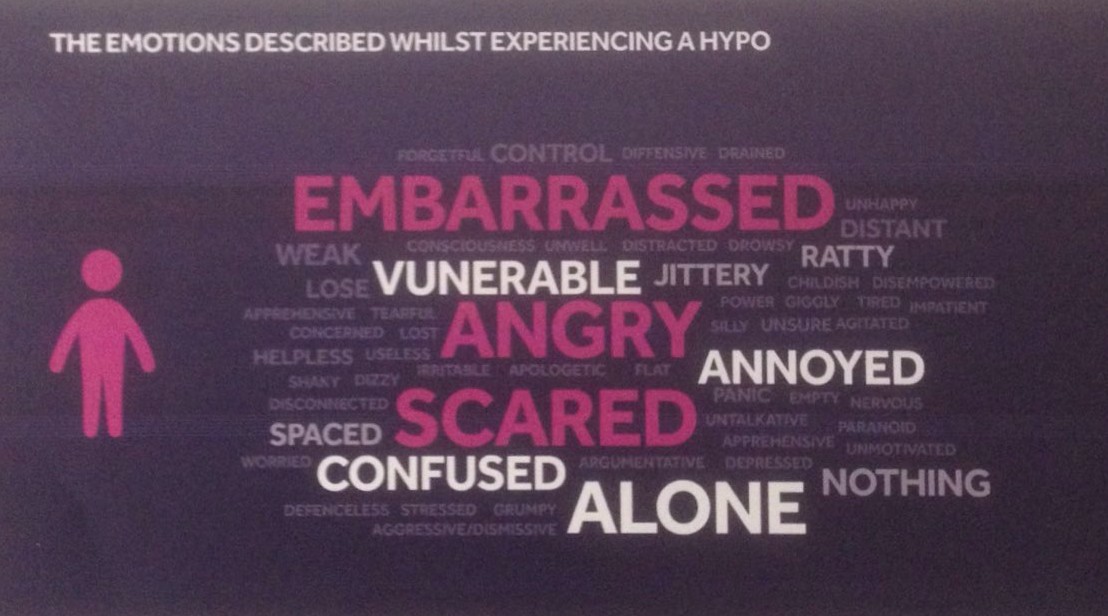
- I held off on exercising until I got my insulin pump and my children starting school made this easier too. My resistance was due to fear or unwillingness to deal with the initial hypos while on multiple daily injections (MDI). However, the more I read about the longest living people with type 1 diabetes, the more I realised that exercise seemed to be one of their key elements to good control. Plus, when my joints started to get achy that was an added incentive.
- Attend multiple medical appointments:
- I used to see my endocrinologist 3 times a year, but this seems to be reduced to oncer every 8 months. I’m not sure how I feel about this. I also visit a podiatrist & optician annually through the National Diabetic Retina screen programme and the community podiatry service.
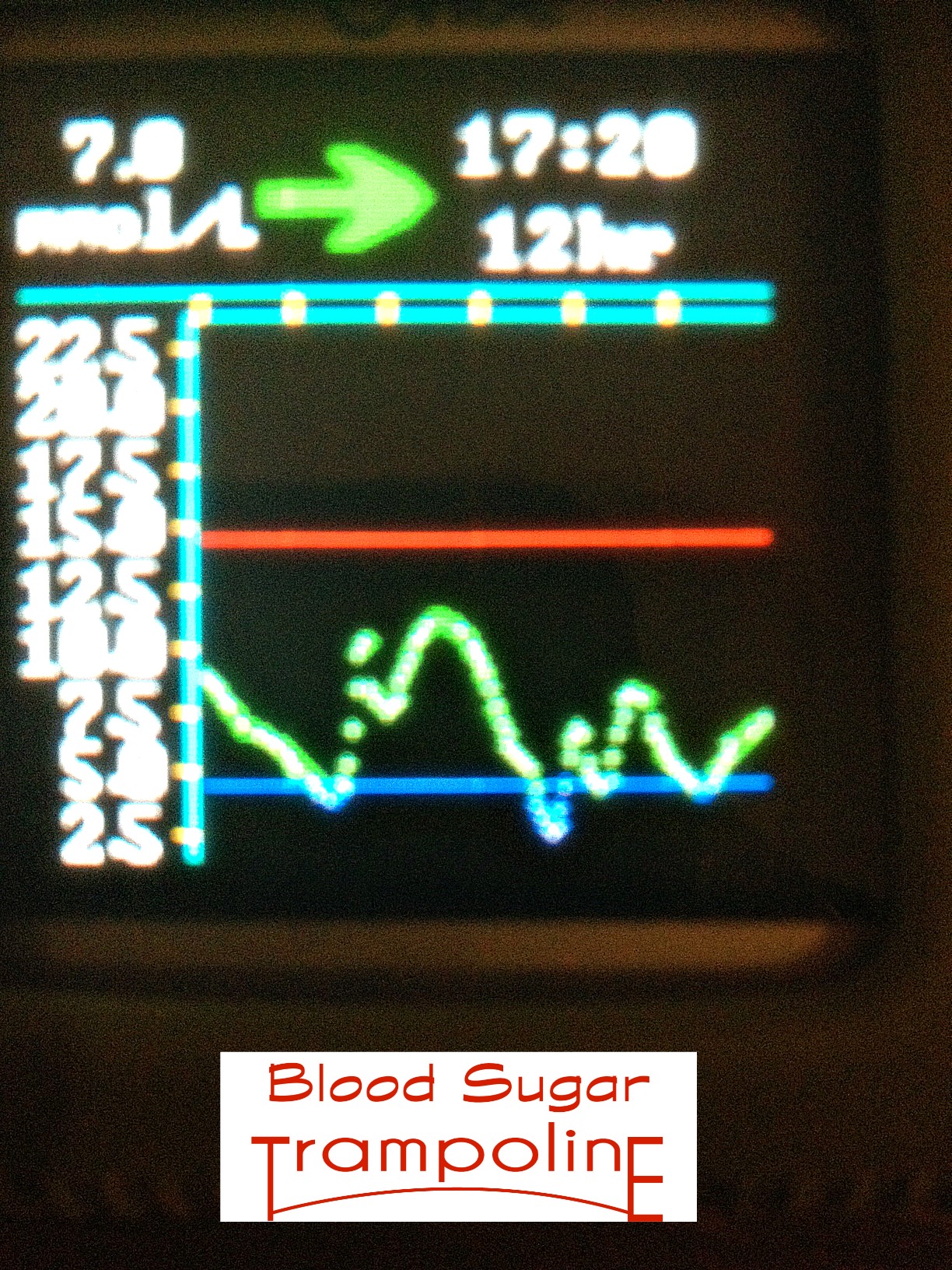
- Upload my insulin pump and CGM data to a computer programme:
- I do this at least once every three months and definitely before a clinic visit.
- Prepare thoroughly for my clinic visit:
- by having my blood work done well in advance, I collect the lab report from my GP and keep a copy for my own records. I make a note of any questions I want to ask and make sure that I have time to ask it.
- A good support system is important to me.
- My husband is crucial in this; he needs to understand diabetes as much as I do. I’m also a member of a Type 1 Support group and I draw comfort from meeting others just like me who speak my language. I also participate in many diabetes online groups.

- My husband is crucial in this; he needs to understand diabetes as much as I do. I’m also a member of a Type 1 Support group and I draw comfort from meeting others just like me who speak my language. I also participate in many diabetes online groups.
- Making sure I know as much as I possibly can about my diabetes;
- I draw motivation from reputable diabetes websites that I can relate to and by reading stories like that of Bob Krause who lived in San Diego and at the age of 90 has lived with Type 1 diabetes for 85 years and is still hale and hearty. I read about Nat Strand who won The Amazing Race, Charlie Kimble race car driver.
- Making time for all things diabetes related while not letting it take over my life.
Diabetes is frustrating at times but I’m not about to give up. I’ll give it my very best because I have soo much to live for. All of this may sound like it consumes a huge amount of my time but the more you do it the less time it takes.