The HSE discriminates against people with type 1 diabetes on the Freestyle Libre reimbursement scheme announced on January 19th 2018. The HSE states that it bases it recommendations on the Health Technology Assessment Group (HTAG) Advice Note so “that numbers being treated do not exceed that expected”.
The HTAG Advice Note recommends that:
“Careful patient selection should be part of the agreement, with hospital consultant initiation, and preference for children and young adults in the first instance so that numbers being treated do not exceed that expected, despite the lack of clinical evidence that the Freestyle Libre is beneficial for this group.
I completely support taking a phased approach to this scheme as nobody knows how much it’s going to cost or save and this is a brand new scheme that will need to be tweaked.
Service Providers Must Make Reasonable Accommodations
However, there were many, many, many ways the HSE could have found to phase in the Freestyle Libre, in addition to clinical need but not limited by age. I can think of three straight away that would also not not allow the numbers of users to exceed expectations.
In fact, “The law which deals with disability in the provision of goods and services is the Equal Status Acts 2000-2015 (ESA) “says that service providers must make reasonable accommodations so that people with disabilities can use services like everyone else (Source - Human Rights Equality Commision).
I would actually argue that a person growing a tiny human in their dysfunctional body or a person who is on the verge of developing diabetic complications should be included.
Maybe a person with a medical card who would otherwise never afford this device should be prioritised?
Or person who is required to do SMBG testing "more than 10 times a day if this is necessary because of the person's lifestyle (for example, driving for a long period of time, undertaking high-risk activity or occupation, travel)." Source: UK NICE Guidelines. The NHS have issued similar guidelines to the Regional Medicines Optimisation Committee (RMOC) on who should be reimbursed for Flash Glucose Monitoring Systems.
Lacks Clinical Evidence to Support Recommendations
The HTAG document makes it’s recommendation that this device be approved for children without any clinical evidence to support it.
It completely contradicts itself by saying that none of the clinical trials used to based their recommendations on had children as participants, that they are “unclear whether data from these (clinical trials Bolinder et al. 2016; Haak et al. 2017) trials are generalizable to children.” The HTAG acknowledges that “There is limited data to support the routine use in people who are less well managed or in children and young people.”
Yet this is the group they recommend. The HSE have chosen to ignore the clinical evidence from two clinical trials of the many, many benefits to adults on MDI.
“Careful patient selection should be part of the agreement, with hospital consultant initiation, and preference for children and young adults in the first instance so that numbers being treated do not exceed that expected.”
They also chose to ignore the Expert Opinions who:
“consider the product would be of benefit to all patients with diabetes using multiple daily injections, however those who would benefit the most include:
- Young people with type 1 diabetes
- Parents or carers of children with type 1 diabetes
- People who struggle with SMBG
- People who lead active lives
- People who have poor hypoglycaemic awareness”.
Continuing Discriminatory Pattern towards Adults with Type 1 Diabetes
This is not the first time that the HSE have discriminated against adults with type 1 diabetes. Adults have been excluded from standard access to insulin pumps and from standard diabetes education so “that numbers being treated do not exceed that expected”. And now, the Freestyle Libre.
When will the 13,000 Adults with Type 1 diabetes have the same provision of medical devices and services as children with type 1 diabetes?
When will our HSE and our government stop viewing us as a financial drain on the healthcare budget and finally see adults with type 1 diabetes as people worth investing in?
The HTAG document was published on the 11th November 2017 and can be found here. As of 3pm Thursday 15th February, this document has been taken off he HSE website, if you would like to view it you can do so here.
I posted my initial reaction to the HSE’s announcement here if you need background information.
See this post from Thriveabetes on what is happening with the Equality for all People with type 1 diabetes campaign.









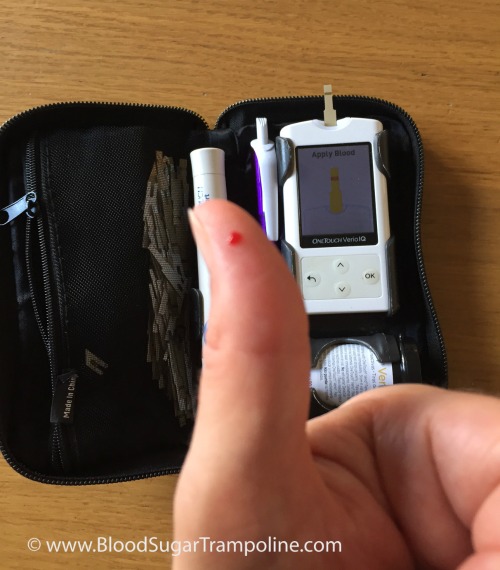
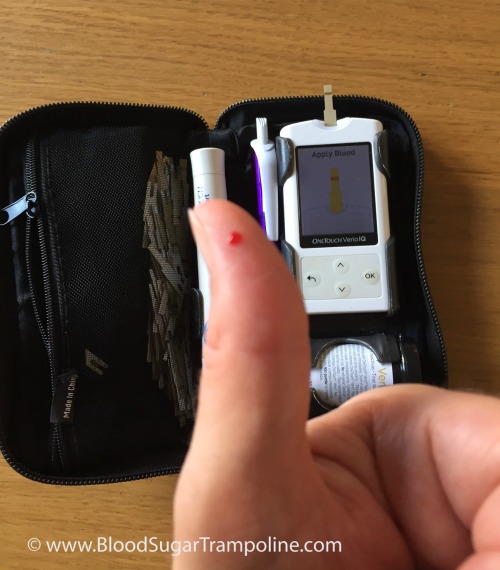 Before breakfast, I checked my levels again; they were in target, so I took my insulin for my regular weekend breakfast of tea and toast also known as 40g of carbs and then ate it.
Before breakfast, I checked my levels again; they were in target, so I took my insulin for my regular weekend breakfast of tea and toast also known as 40g of carbs and then ate it.